An ever-increasing diversity of street drugs makes it challenging to quantify the risks
“Bath salts”, “plant food” and even “research chemicals” are some of the terms an expanding array of new, usually illicit, drugs are advertised under.
But these innocuous-sounding labels belie the more alarming coverage they get in the media, when they are linked to high-profile overdoses. Instead of more familiar names, such as heroin, ice and MDMA, these drugs are more likely to go by a string of numbers and letters.
The major problem with many of these drugs is their novelty. They are mysterious, even to the doctors and researchers that study them. And education is a two-edged sword, the experts say.
“If you run a mass media campaign about a drug that most people haven’t even heard about, you create interest where no interest existed before,” Professor Steve Allsop from the National Drug Research Institute says.
In contrast, GPs can provide much more targeted information about risk.
Part of this is understanding the new and emerging drugs which are out there, and what drives individuals to use them.

What are they?
New or novel psychoactive substances, known by researchers as NPS, is a bit of a fuzzy term. It has been defined by the European drug monitoring body as anything “not controlled by the 1961 Convention on Narcotic Drugs or the 1971 Convention on Psychotropic Substances, but which may pose a public health threat”.
However, this failed to capture the growth in popularity of older drugs such as DMT and 2C-B, so researchers came up with “emerging psychoactive substances”, or EPS, to capture both these and the newer drugs.
Often sold as “legal highs”, these drugs can be broadly split into four categories: the cannabis-type substances; the stimulant-type substances like “bath salts” and “meow meow”; the hallucinogen-type substances such as NBOMes; and the group that’s particularly concerning some health professionals, fentanyl-derivatives.
While they were first popular among the psychonauts and party crowd, these drugs are increasingly being used by chronic and marginalised drug users and by people seeking to self-medicate. Many consumers seek them out as replacements for traditional drugs such as cannabis, heroin, amphetamines, MDMA, benzodiazepines, LSD and cocaine.
A fundamental problem in understanding the use and harms around these drugs is the lack of hard data. In the 1990s, the “godfather of psychedelics” chemist Alexander Shulgin published two books detailing the synthesis and effect of hundreds of different compounds, but many more drugs have been developed since then.
In the last decade alone, EU drug monitors recorded a jump from a dozen to 100 previously unseen psychoactive substances on the market that year between 2005 and 2015. Currently, the EU drugs agency tracks more than 620 psychoactive substances, although the development of new drugs appears to have slumped, with only 66 coming on its radar last year.
A major difficulty for both law enforcement and public health is that they often have little idea of what active drug is in the product until it gets tested, and that can vary from batch to batch, Professor Allsop says.
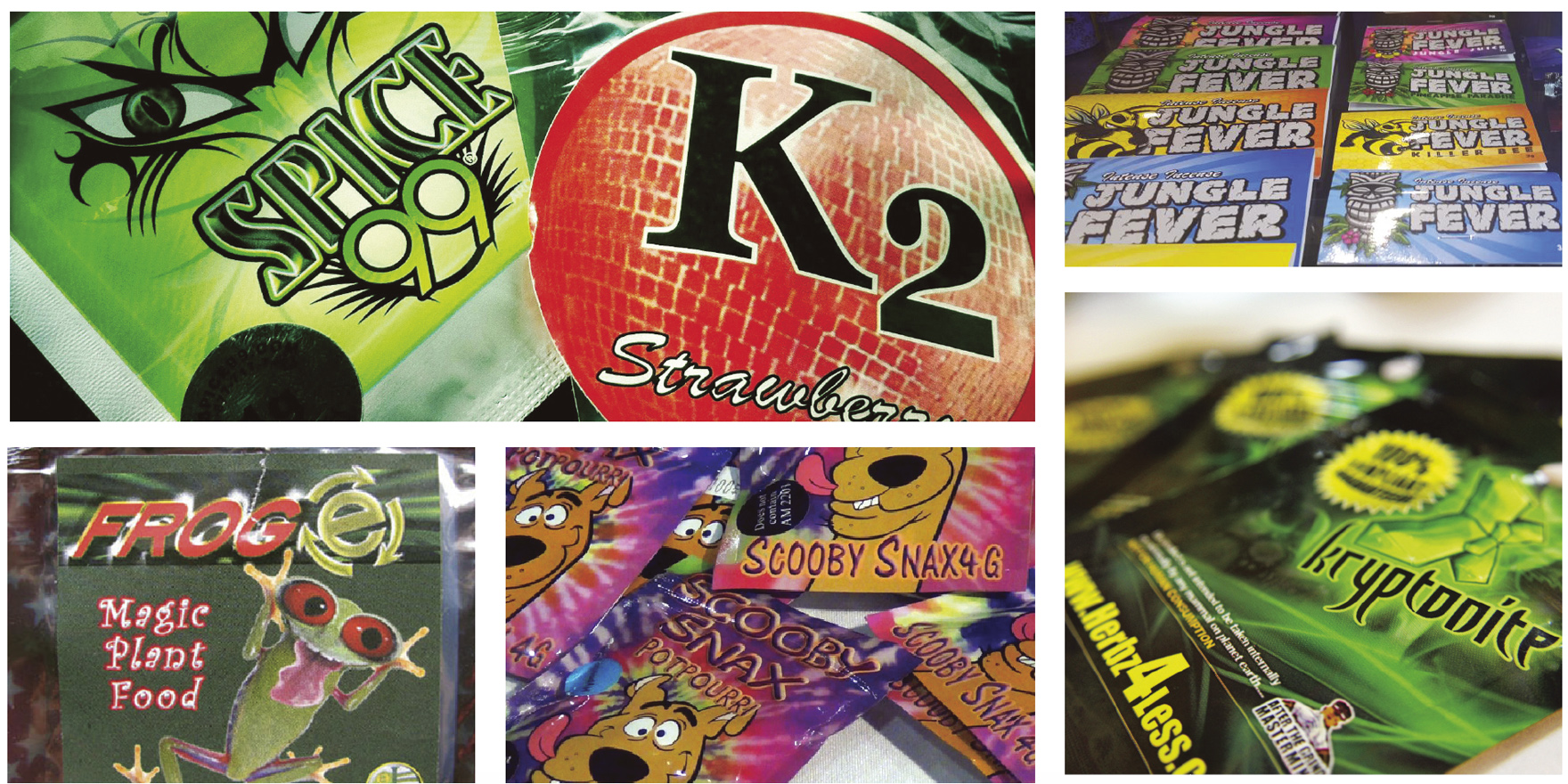
One illustration is the synthetic cannabinoid, Kronic, which only appeared in Europe in the early 2000s and mid-to-late 2000s in Australia. The synthetic cannabis sold in shops and online is in brightly coloured and professional looking packets, and includes plant matter that has been sprayed with chemicals from the manufacturers.
While claims are made on the packet about the type of high the product will induce, it’s often unknown, Professor Allsop says.
Being a legal way to get high was a major part of the early appeal for many users. And before a ban was put on all synthetic cannabinoids in many parts of the world, manufacturers would be switching formulations to constantly stay one step ahead of law.
Professor Allsop gives an example of when one of the earlier formulas for Kronic was banned in Western Australia, and the manufacturers simply brought out another version and advertised it as a new formula that was “totally legal”.
“The nature and the potency of these products change from time to time, and therefore the risks change from time to time – and that doesn’t include individual vulnerabilities that people might have,” Professor Allsop says.
“When [synthetic cannabis] first appeared on the market we knew very, very little about the short-term effects, and in fact, even now much of the evidence is based on very small clinical samples and self-reports from the consumers.”
Much of the research has been done on small sample sizes, some as little as nine to 15 people, and a major challenge is actually determining what people took. If researchers are asking people to self-report, how do they know if what the participant think they consumed is what they actually consumed, he says.
“We know very little about the short-term effects and we know nothing about the long-term effects.”
Nevertheless, it’s not as if hundreds of psychoactive substances are flooding the streets of Australian towns. Most of the products don’t gain a foothold because users simply don’t like their price, side effects or high compared with other drugs already available, Professor Allsop explained.
Only a relatively small proportion have any staying power.
This is illustrated by Australian research, which first started tracking consumption of these substances across the population in 2013 as part of the National Drug Strategy Household Survey.
By 2016, more people in the population had tried synthetic cannabinoids at some point in their lives, doubling from 1.3% to 2.8% since 2013.
But when you look at people who had recently used synthetic cannabinoids such as Spice and Kronic, the story is different. Only 0.3% had used the drugs recently in 2016, down from 1.2% of the population in 2013. The Australian Institute of Health and Welfare interpreted this to mean that “while people may have experimented with this drug since 2013, most choose to no longer to use them in 2016”.
Meanwhile, the proportion of the population recently using other emerging psychoactive substances, such as DMT and mephedrone, remained relatively stable at only around 0.4%, or 60,000 people.
“It is important to note that frequency of these drugs remains low,” says Rachel Sutherland, a researcher at the National Drug and Alcohol Research Centre who tracks the use of both new and emerging psychoactive substances.
She says most of those who reported using these drugs said they only used them for a median of one or two days in the past six months.
“Much of the risk among this group seems to come from their polydrug use [i.e. using multiple different drugs] rather than from their [psychoactive substance] use per se.”
Why do people use them?
Ms Sutherland and her colleagues at the National Drug and Alcohol Centre teamed up with researchers at the National Drug Research Institute to find out what drew users to these new and emerging drugs.
In a paper published earlier this year, they explained that the availability and legality of drugs such as synthetic cannabis and cathinones such as “bath salts” were the major drivers for Australian users.
As well as their perceived legality, one of the big drivers towards new psychoactive substance use has been workplace testing, according to John Ryan, CEO of the Penington Institute, group that promotes evidence based policy and practice to reduce drug-related harms.
People are shifting from cannabis to synthetic cannabis or methamphetamine because cannabis can be detected in the system for longer, he says.
“People have switched from drugs that are detectable through the testing methodology toward drugs that will allow them to avoid testing,” Mr Ryan says. “So, we’re actually shifting people from a less dangerous drug to a more dangerous drug.”
“[Also], these synthetic drugs are much easier to manufacture than plants that are grown in the ground and subject to crop cycles, flood and drought like traditional … cannabis,” Mr Ryan says. They can typically be manufactured in days rather than months.
The drugs are more potent, take less space to manufacture and harder to detect with drug-testing – a clear incentive for those in the trade.
Manufacture has become widespread, from sophisticated factories to backyard labs.
For users, being able to go to a professional-looking website and purchase the drugs with a credit card made drugs like synthetic cannabinoids appealing, Professor Allsop says.
But the recent change in legality has made it less attractive, and users are reporting a dislike for the side effects and the expense, which may explain the drop off in use.
Some workplaces are now testing for synthetic cannabinoids as well, further limiting their appeal.
On the other hand, Ms Sutherland’s research found that the psychedelic drugs in the NBOMes and the 2C-x classes were prized for their value for money and because users tended to view them as having a better high and level of purity compared with traditional alternatives such as MDMA and LSD.
A big bust, and subsequent global shortage, of MDMA in the mid-2000s is also thought to be one of the factors leading to the adoption of cathinones, such as mephedrone, that were first slipped in to mimic MDMA and later became popular in their own right.
Some fulfil the same demand that empathogenic and entactogenic drugs, such as MDMA, do, which is the feeling of love and connectedness to others and the world, but have the drawcard of a cocaine-like effect as well.
But the survey found that a major motivator for use of mephedrone, the most commonly used cathinone, was availability. This suggests their use may drop off if more appealing alternatives, such as ecstasy and cocaine, remain available, Ms Sutherland and her colleagues say.
Because of the underground nature of both traditional drug use and new psychoactive-substance use, it’s not clear how often people buy them thinking it’s another drug.
But it is rare that consumers buy illicit substances that are 100% pure anyway, Professor Allsop says “and even if it was 100% pure, it still carries risks”.
While it’s often difficult to give clear advice on what each drug will do, doctors can advise that they may demonstrate similar potential for harms as the drugs they mimic, he says.
Some of the effects from synthetic cannabis are similar to what you might get from cannabis, he says, “but they also demonstrate sometimes significant variations in potency and, of course, that increases the potential for misdosing or overdosing”.
“What you bought this week might be quite different from what you bought last week,” he says. “By their very nature, there’s no quality control.”
It may be fruitless to try become an expert on the hundreds of different products out there, because unfortunately, when it comes to adverse effects, pinpointing which drug might be the culprit will often be difficult.
“The precision to give that sort of advice is lacking,” Professor Allsop says.
“We don’t know what these substances are, and even when we do know what they are, with a lot of the new psychoactive substances we have an imperfect sense of what the acute risks are, and we certainly have very little evidence about the chronic risks,” he adds.
While we lack quality evidence for many of the drugs out there, Professor Allsop said that we can make an assumption: “if a drug is being marketed as having similar effects as cocaine or cannabis, then we can at least make an assumption that it may have at least some of the similar adverse risks.”
In this way, risks associated with taking stimulants while having high blood pressure, or fentanyl derivatives while also on prescription opioids, would be known.
“But we can also potentially assume that it may be more risky.”
Mr Ryan says telling people to “just say no” to these drugs is unlikely to work. “You’ve got to actually understand what’s happening in their world, and also to gently try to nudge them towards a more healthy approach”.
That would obviously be to not take them at all, but if they choose to, then to use as little as possible and as least often as possible.
“Some more cheeky doctors would probably even say to their patients, don’t use synthetic cannabis, use the original cannabis – at least we know what the consequences of that are.”
According to Mr Ryan, stamping down on illicit drug us, and approaching it through a criminal lens has spawned more unknown quantities in the community as people creatively adapt.
“We’ve gone from much lower potency amphetamine to … more potent amphetamine imitators in the [new psychoactive substances] category,” Mr Ryan says.
“And, generally, in cannabis we’ve gone from much less potent cannabis to much more potent cannabis in the last 20 years under the criminal system. And now we’ve got lots of cannabis imitators which are probably even more dangerous than the highly potent plant-based cannabis.”
“The problem is that we’re seeing an ever-increasing diversity of drugs, and a shift toward even more powerful and more synthetic drugs – and that’s basically the [new psychoactive substance] story.
“It’s a result of our failure to properly manage drug consumption.”