The RACGP provides five top tips for prescribing nicotine vaping products for smoking cessation, including example prescriptions.
The RACGP has released its long (eight months by our calculations)-awaited guidelines for smoking and vaping cessation.
Supporting smoking & vaping cessation: A guide for health professionals centralises the current information on the regulation of access, prescribing and minimum product standards for vaping products.
It reviews the risks and efficacy of vapes as smoking cessation aids, as well as the efficacy of other approaches and guidance for vaping cessation.
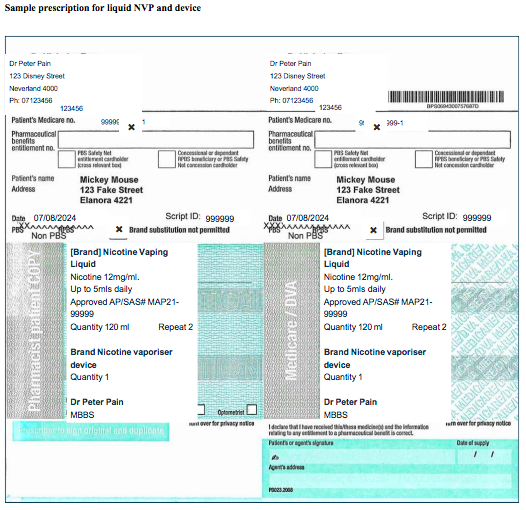
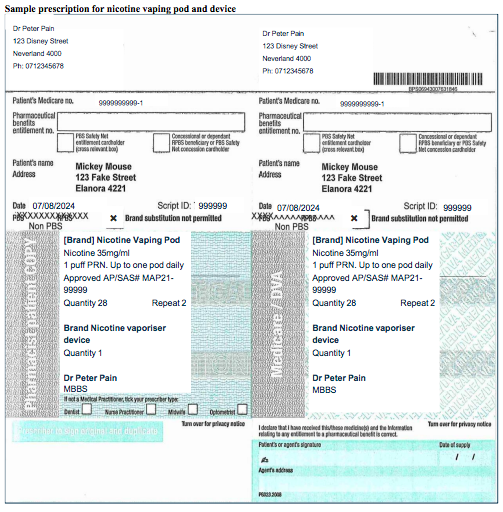
In practical advice, the guidelines outline how to write a vape prescription, with examples.
Prescriptions should include the brand and product (although this is not essential), nicotine concentration (in mg/mL), recommended daily dose, initial quantity and repeats, and the Authorised Prescriber number or the SAS approval/notification number (if using either access pathway).
The flavour can also be specified.
The college provided five top tips to minimise the risk of harm, as nicotine vaping products (NVPs) remain unregistered.
Firstly, the RACGP recommended that “premixed ‘closed’ systems” devices should be preferred to open devices that use liquid nicotine, particularly for new users.
This minimises the risk of poisoning or toxic exposure.
“If you are prescribing for an experienced user, you may consider any preferences they have for a vaping device and/or liquid; however, pharmacists will only be able to dispense a vaping substance in final dosage,” the guidelines say – meaning they cannot dispense component ingredients for consumers to use to mix their own substances.
“Pharmacists will only be able to dispense vaping products included in the TGA’s list of notified vapes.”
Speaking to The Medical Republic, RACGP addiction medicine special interest group chair Dr Hester Wilson encouraged GPs to discuss available products with their local pharmacists and to avoid Big Tobacco-made products where possible.
The guidelines recommend against prescribing free-base liquid nicotine at concentrations over 20mg/mL, as these require dilution and increase the risk of poisoning.
Thirdly, they recommend limiting the supply per script.
“The RACGP expert advisory group recommends limiting the prescription to a maximum of three months’ supply and arranging a follow-up appointment that coincides with the expiry of the prescribed amount,” the guidelines say.
“This could also be earlier if required, e.g. [by] a younger patient.”
Where possible, avoid flavourings, the document says.
Dr Wilson said there was some evidence to suggest menthol vapes were harder to stop.
In its fifth tip, the college encourages follow-ups and behavioural support alongside prescriptions.
“The role of the GP and/or nurse practitioner is important in providing follow-up and ongoing support to assist with successful cessation,” it says.
“Consider also referring patients to Quitline.”
The guidelines say to choose a starting dose based on the patient’s level of nicotine dependence, while acknowledging that the evidence remains scant.
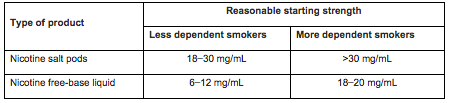
“When prescribing for current users of NVPs, consider any preferences they have for concentration, device, and daily use; however, supply can only be those on the TGA list of notified vapes. It will be important to speak to the pharmacist to determine availability of supplies.
“If the patient is currently using an open system device and moderate to high nicotine concentration, reduce the risk of poisoning by recommending they change to nicotine free-base with a concentration of ≤20mg/mL and/or a closed system device in order to avoid the risks involved in dilution of nicotine liquid.”
The guidelines outline requirements for clinical note-taking: justification, confirmation of informed consent and any adverse events.
“The TGA vaping hub stated [informed consent] needs to be in writing for the AP scheme,” read the guidelines.
“It is good practice to obtain written, signed informed consent for all unapproved medicines.”
Beyond the use of vapes for smoking cessation, the guidelines also tackle vaping cessation.
The college recommended the three-step and five-step brief intervention approaches: “ask, advise, help” and “ask, assess, advise, assist and arrange” respectively.
A more expansive breakdown of the intervention can be found from page 24 of the guide onwards.
Dr Wilson pointed to the new AJGP paper on assisting young people quit vaping in general practice.
The RACGP’s guide also covers the use of pharmacotherapies for vaping (page 28) including nicotine replacement therapies, varenicline, cytisine and bupropion.
Dr Wilson said the key takeaway was that the name of the game was nicotine cessation.
“It’s not about ongoing access to nicotine,” she said.
“While [vapes] are unapproved, there is a process for prescribing them, and ideally it needs to be within the whole focus of nicotine cessation … but it’s also about harm reduction.
“There certainly will be some people where, as much as I would love them not to be using e-cigarettes, it’s probably better for them to be using e-cigarettes than to be smoking tobacco.”
Related
Dr Wilson said that while the guidelines didn’t directly comment on how to navigate requests for prescriptions where the goal didn’t appear to be cessation, GPs should engage in honest conversations and aim for harm reduction.
“The advantage that we have in general practice is we know our patients, we know their families, we know their social setup and the challenges that they face, and we can work with people over time to shift where they’re at with [vaping],” she said.
“But it is a tricky one.
“If you’re providing a prescription and you’re thinking, ‘this is not actually about cessation’, are [you] comfortable that for this individual it’s actually about harm reduction?
“It’s a nuanced area.”
Dr Wilson said the advisory group had aimed to create guidelines that were “pragmatic” and supported both GPs who wanted to be able to prescribe vapes and those who chose not to.
She added that with the ongoing fluctuation in regulation – here’s looking at you Tasmania and Western Australia – it had been tricky to provide all encompassing guidance, but that the document would remain “living”.