A Medicare expert pulls apart the latest set of legislative amendments and finds little for doctors to celebrate.
A bill to amend legislation governing the Professional Services Review does nothing to fix the structural problems in the system, says an expert in Medicare law; instead it plugs holes that have caused the PSR trouble in court.
It also lowers the threshold for referrals; expands the PSR’s reach to doctors who have not been referred; increases debt-recovery powers; and promises educational “counselling” that no one is qualified to provide.
Dr Margaret Faux, a health system administrator with a PhD in Medicare compliance, says the Health Legislation Amendment (Medicare Compliance and Other Measures) Bill 2021 is like “fixing the windscreen wipers on a car when the engine is faulty”.
“This is the wrong approach,” Dr Faux tells TMR. “What we have is an outdated pay-and-chase model that is ineffective.
“If the penalties for drink-driving offences were suddenly doubled, when it was well known that the breathalyzer equipment gave inaccurate or inconsistent results, there would be public outrage. And that’s what we’ve basically got here: we’re giving more power to a secret agency, when we know that the underlying equipment, [Medicare legislation], is completely faulty, and unable to be interpreted.
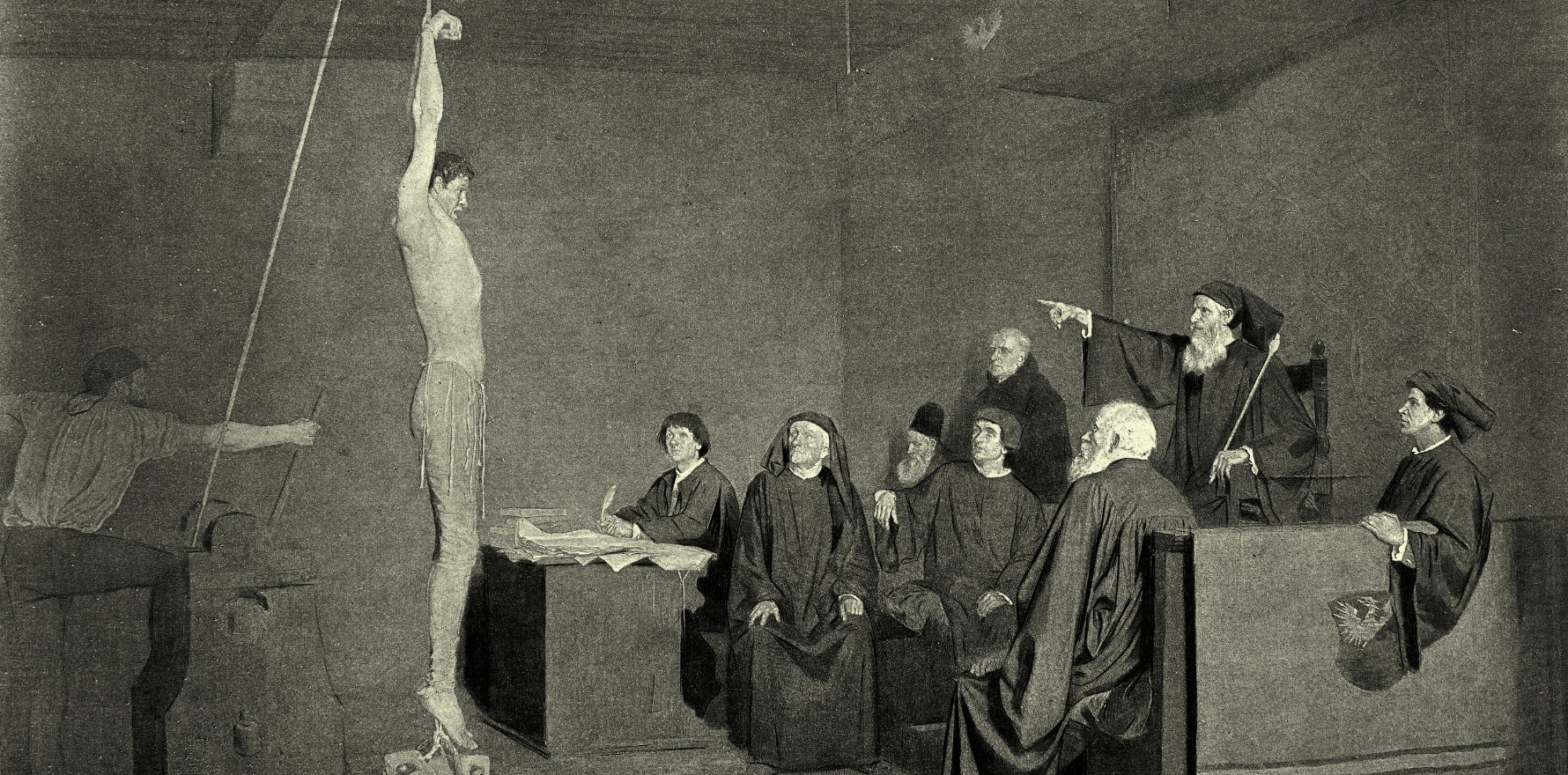
“So I predict that there will be more and more litigation against the PSR, and more doctors will rebel against this draconian system that is really becoming more and more medieval.”
The bill now before parliament is the fourth set of amendments to the legislation since 2018.
Here are Dr Faux’s interpretations of some of the main changes.
- New power for the Director of PSR to enter into agreements with corporate entities
Corporates taking more of the flak may sound like a good thing, if you recall our coverage of Dr Hamid Norouzi’s Federal Court case. He was one of three doctors targeted by the PSR for billing while working for House Call Doctor, a mostly after-hours service in Queensland. The three doctors claimed they had little or no control over their claiming and paid half their billings to the company, but were left to foot their huge PSR bills alone.
But this amendment probably has more to do with the National Home Doctor Service, which succeeded in getting the PSR’s case against it set aside.
“This is plugging holes where the PSR has failed in the Federal Court,” Dr Faux says.
“But I expect that there will be more litigation, because corporate stakeholders have the capital to fight this type of heavy-handed approach by the government.
“In the end, the department wants the money back, and they don’t care where they get it. The only place they can get it from is the bank account into which it was deposited. That’s why they come after the doctor.
“But of course, corporatisation of medical practice means the money can be deposited into a different bank account before being distributed.”
The AMA, however, says the amendment really is there to make corporates take more responsibility.
“The AMA have been informed that this legislation is designed to address the Government’s concerns about potential gaps in compliance powers, including the inability to enter into s92 agreements with corporate entities,” vice president Dr Chris Moy tells TMR.
“The AMA has been in support of extending the option s92 agreements to apply to corporate entities instead of just the individual doctors as is the case now. The concern has arisen in particular where issues have been as a result of the corporate entity rather than the individual.
“Through consultation with the Department of Health the AMA has ensured that there are additional protections in the Bill to protect individual practitioners subject to compliance activities and believes the Bill is a better Bill than originally proposed.“
- Counselling and education
Under “Changes to the types of specified actions which can be taken under an agreement”, the bill provides for the Director or her nominee “to counsel the person under review. Counselling focuses on education … and is intended to prevent future inappropriate practice by ensuring that the person is aware of what is expected of them and how to correct past behaviour.”
Many GPs would welcome such education, if they could depend on it. But this gets to the heart of the problem with Medicare: there are no fixed, written standards for appropriate use of a highly interpretable legal instrument; doctors are never trained in how to apply it; and there is no one whose job or qualification it is to educate them.
“Who’s going to provide that education?” asks Dr Faux. “We don’t have any medical billing experts in Australia – that category of person does not currently exist.
“Some of the colleges say it’s the medical defence organisations’ job, but really it’s not their job to interpret Medicare law.
“We’ve never had a national curriculum on this topic. What you’ve got at best is people with varying levels of self-taught knowledge, including inside the department, and the department is known to give incorrect education and advice.
“You can’t do counselling around education, until you first write the rulebook.”
- Accessing records of non-referred practitioners
In passing, the bill digest mentions that “the PSR may access the records of health practitioners who have not been referred to PSR in determining whether a practitioner who has been referred is engaging in inappropriate practice”.
“This is very important,” Dr Faux says. “And in my view, very worrying. The Director can request records from a practitioner who’s not under review, but may have referred a patient or seen a patient [also in the care of a referred doctor]. I think that is designed to capture provider number sharing, which is not permitted and is absolutely inappropriate behaviour. But a better approach is just to teach doctors that.
“This enables them to investigate much more widely and look at referral pathways as well, to see how these patients are being passed around and who’s claiming what for what patient. I think that is very worrying and it may also be a privacy breach, because you’re asking doctors who are not referred to hand over patient records.
“Why are we casting the net this wide?”
- Expanded debt-recovery powers
Among the bill’s amendments on this front are ones that “expand the situations in which the Commonwealth can seek to recover payment from a deceased person’s estate” and “expand the application of existing financial gathering information powers in the HIA to a wider range of scenarios”.
The problem with this, Dr Faux says, is the lack of any objective, legal assessment of whether such a debt really is owed to the Commonwealth.
“If they say there’s a debt, there’s a debt,” she says.
On a similar note, Dr Faux takes issue with the claim in the digest that in 2018-19 the Department of Health recovered “$49.3 million in claims which should not have been paid”.
“We do not know that $49.3m should not have been paid,” she says. “There is no proof of that. It is equally possible that much of that $49.3m should have been paid, that it was legitimate claims, but that the doctors decided to acquiesce to what they perceive to be coercive demands for repayment around a system that they don’t understand. They don’t know whether they’ve done anything wrong, but they want the problem to go away.
“The fact that the department says a claim should not have been paid, does not make that legally correct.”
- Clarifications of the role of the Chief Executive of Medicare and Director of the PSR
The explanatory memorandum to the bill says “that there is no requirement for the CEM to undertake an investigation to objectively determine that a particular person provided services and/or engaged in inappropriate practice, prior to making a request to the Director”.
It also clarifies that it “has never been part of the PSR scheme that the Director makes any findings in relation to inappropriate practice before referring a matter to a PSR Committee”.
“What that means to me is that the chief executive of Medicare has less work to do: they can use their algorithm to determine that someone is an outlier and just refer them straight to the PSR without even bothering to look at it,” Dr Faux says.
She says the obligation for the Director to have made a finding before referring to a committee is another aspect that has been contested in court, and that this amendment plugs that gap. “It’s bolstering the powers of the agency, without giving any reciprocal rights to the person under review.”
Reviewing the Reviewers
According to a report in The Saturday Paper, ANU administrative law expert Professor Robin Creyke is leading an independent review into section 92 agreements.
AMA vice president Dr Chris Moy says the review comes at the AMA’s instigation.
“The AMA had previously made representations to the Department of Health and the Minister for Health calling for a review of the process following concerns raised by members,” he tells TMR.
“The s92 independent review that has been established is a direct result of these representations and will be able to examine concerns raised about the process and determine what improvements might be needed to ensure it is fair and transparent.”
But Dr Faux says that even with a professor who is highly skilled in administrative law, without taking in the whole context – namely, that the regulations are not comprehensible and that there is nowhere for GPs to go for reliable education – a review of S92 agreements is likely to be superficial.
RACGP president Dr Karen Price advised GPs last week to privately bill as many patients as possible, saying high levels of bulk-billing – nearly 90% of services to use the Health Minister’s figure – left them with no bargaining power.
Dr Faux disputes the cited figure, and says the true percentage of fully correct and compliant bulk-billing is, somewhat shockingly, closer to 20% of services.
But she agrees GPs should take the advice, not for political reasons, but for their own safety.
“Bulk-billing was intended to be a benefit to doctors and patients: certain, immediate payment, albeit at a lower amount, would enable you to run a practice; and patients didn’t have to pay out of pocket,” she says.
“But any perceived benefits of bulk-billing and no-gap claiming have been now overtaken by a corresponding threat of being audited and investigated and having to pay all the money back. So we’ve shifted the cost burden to consumers, not necessarily because doctors want to charge their patients more, but because it’s safer.
“We’ve completely messed it up,” she adds, referring to Medicare’s worthy project of universal healthcare.
“[This bill] is tinkering and putting the cart before the horse, and it’ll have a negative impact on patient care.”