Uncommon side effects – a case study.
Mrs M, in her late 60s presented with abdominal pain and weight loss. CT scans showed a lesion in the pancreatic gland. Biopsy of the pancreatic lesion revealed adenocarcinoma.
Her cancer was deemed borderline operable, given the involvement of superior mesenteric artery.
Further imaging with CT and PET scans showed another lesion in her right lung. It was biopsied and confirmed as adenocarcinoma of the lung.
Mrs M was fit and well despite two primary malignancies, a lung cancer and a pancreatic cancer.
Conversion chemotherapy with gemcitabine and nab-paclitaxel was chosen as the treatment option to convert her borderline-operable pancreatic cancer into an operable cancer. This particular regimen was thought most appropriate because of the known activity of gemcitabine and nab-paclitaxel on both lung cancer and pancreatic cancer1,2.
The treatment regimen comprised both agents being given weekly for three weeks in four-weekly cycles3,4.
After two cycles of chemotherapy, the patient started experiencing calf pain and weakness.
Examination revealed tenderness and swelling in her lower limbs bilaterally extending from the hip downwards, more prominent in the thigh area. The patient became wheelchair-bound, mainly because of pain. Examination did not reveal any neurological deficits.
Chemotherapy was stopped because of poor performance status.
Blood tests showed creatinine kinase level of 400. Even though CK levels were elevated, rhabdomyolysis is generally associated with much higher levels than these. The patient did not have any other features of rhabdomyolysis such as fever, gastrointestinal symptoms or renal failure.
An MRI scan was performed and this showed diffuse inflammation in her calf muscles. Patient was unable to mobilise because of pain and weakness.
Muscle biopsy was thought necessary to aid diagnosis and Mrs M was transferred to a tertiary centre for this procedure.
Due to the severity of her condition, and after consultation with rheumatological team, the patient was started on prednisolone.
Chemotherapy was ceased because of her poor functional status.
Following the cessation of the chemotherapy, the patient recovered rapidly, and full recovery was achieved in three weeks.
Myositis caused by gemcitabine was considered the likely cause, given the close chronological association and the lack of other possible causes.
The patient later went on to have fluorouracil- and oxaliplatin-based chemotherapy without recurrence of her myositis.
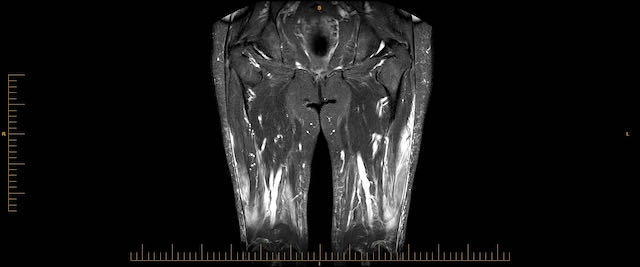
Imaging findings (see image above)
MRI shows extensive bilateral quadriceps myositis involving mid to distal segments. PET scans also show FDG uptake in the quadriceps muscles.
Discussion
Patient did not have history or investigation results suggestive of inflammatory conditions such as dermatomyositis, polymyositis or lupus.
Creatinine kinase levels were high at 400 yet not high enough to consider rhabdomyolysis. Patient was not on any non-chemotherapy drugs that could have contributed to her symptoms.
Out of all the original investigations suggested, muscle biopsy was not performed initially as it required the patient to be transferred to a tertiary care centre to have this procedure. Organising this took a few days. Due to the severity of her symptoms, steroids were started after consultation with the rheumatology team.
Myositis is not a common side effect of gemcitabine.
Current documented evidence is limited to a very few case reports5. The few case reports found on a PubMed search related mainly to gemcitabine-induced, radiation-recall myositis6. There are very few cases of myositis occurring in patients treated with gemcitabine without radiation5.
Gemcitabine should be considered as a possible cause in patients presenting with similar symptoms. Literature review identified a similar case report.
Dr Mihitha Ariyapperuma is a medical oncologist at Icon Cancer Centre Rockingham in Western Australia.
References
1. Lung Cancer. 2013 Jul;81(1):97-101. doi: 10.1016/j.lungcan.2013.02.020. Epub 2013 Mar 30.
2. Gridelli, C., F. Perrone, C. Gallo, et al. 2003. “Chemotherapy for elderly patients with advanced non-small-cell lung cancer: the Multicenter Italian Lung Cancer in the Elderly Study (MILES) phase III randomized trial.” J Natl.Cancer Inst. 95(5):362-372
3. Krishna, K., M. A. Blazer, L. Wei, et al. 2015. “Modified gemcitabine and nab-paclitaxel in patients with metastatic pancreatic cancer (MPC): A single-institution experience.” Journal of Clinical Oncology 1).
4. Von Hoff, D. D., T. Ervin, F. P. Arena, et al. 2013. “Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine.” N Engl J Med 369(18):1691-1703.
5. J Neurooncol 2012 Jan;106(1):15-21. doi: 10.1007/s11060-011-0672-8. Epub 2011 Aug 3.
6. Delavan JA, Chino JP, Vinson EN.Skeletal Radiol. 2015 Mar;44(3):451-5. doi: 10.1007/s00256-014-1996-1. Epub 2014 Sep 6.PMID: 25193536