MyMedicare still lacks a good reason why its two key stakeholders, doctors and patients, will use it.
This is not a “MyMedicare is a bad idea which is definitely going to fail big time” article.
MyMedicare is a solid(ish) idea.
This is more of a “if you look at the fundamentals of MyMedicare so far and how things are starting to unfold in government thinking on the project, it seems to have a lot of design fundamentals and iterating policy characteristics of past big government health project fails – so maybe we should stop for a minute and do a bit more thinking based on what we see so far”, article.
I say this just as some key people involved in helping to run MyMedicare have come up with the idea that we should abandon the basics of building out complex new policy – trials and establishing the proper digital infrastructure, for example – and go faster, with little or no testing or review of where we are, because, well, “it’s urgent”.
In a Q&A webinar on GP Incentives last week, a member of the expert advisory panel said that the panel felt things “just need to get moving” with respect to using MyMedicare as a funding channel.
“This is not an agenda we can be delaying. We all recognise that primary care needs to be supported and be supported now. For that reason, we did not recommend extensive piloting,” one panel member told the webinar audience.
The same panel member – not a doctor or a patient representative – then made a reference to the failure of Health Care Homes, as if that pilot process took just a bit too much time, money and trouble. (Don’t you just hate it when a trial proves your idea fundamentally sucks).
“We actually know an awful lot of what we need to do. We need to just get on and do it by having the appropriate mechanisms and supports for doing so,” said the panel member.
“We don’t want to have another Health Care Homes activity which, due to a whole range of things, was a problematic exercise … not necessarily a negative exercise, but a problematic exercise.
“So … all those who are ready, willing and hungry, get in there, make the best of this.”
Does that mean we can all be confident that, unlike Health Care Homes, MyMedicare is ready to go – no further testing and iterating of any significance required?
The problem is, you could easily argue that the Health Care Homes trials were early version trials of MyMedicare.
MyMedicare is, in one respect, an updated take on Health Care Homes.
So why do we think we “know an awful lot of what to do” all of a sudden, especially given how starkly Health Care Homes failed?
One thing that Health Care Homes warned us about was how wickedly hard it will be to change the behaviour of stakeholders via funding signals alone.
Which brings us to where we seem to be on MyMedicare, which at this point of time feels like a demonstrably confusing place.
So far there is very little incentive for patients to join and not much of an incentive for individual GPs to get involved in a meaningful way either.
No meaningful direct engagement with individual GPs
In last week’s draft recommendations for GP Incentives, a key recommendation was simplification of the PIP and WIP payments into a single practice payment.
That cuts the motivation to engage for most individual GPs out at the get go because they have no direct engagement signal.
And at the practice level, despite what the Incentives Review expert panel intimated to the webinar audience, motivating tenant GPs in a practice to participate is going to get complex and messy because of payroll tax.
The panel suggested there would be no payroll tax problems for a practice or an individual GP, but you’d have to question if the panel, like a lot of other confused stakeholders in the payroll tax debate, do not have their head properly around the complex nature of the payroll tax problem.
For starters, one panel member referred to doctors who might ultimately get some income from a new “simplified” practice payment as “subcontractors”, and then said that as sub ontractors they wouldn’t be seen as employees, so payroll tax wouldn’t be a problem.
Subcontractors is the wrong term to use if the panel was trying to make a reference to “tenant” doctors. Subcontractors mostly are going to be treated as employees by both the ATO and state revenue offices if you understand the detail of what is going on – the correct categories are going to be employees/subcontractors and tenants.
But the bigger problem regarding payroll tax is that the panel seemed to be ignoring what some view as the most important payroll tax ruling in the last year (from the Queensland State Revenue Office), which very clearly says that that one of the best ways for your practice (sorry, administrative entity) to not be levied payroll tax is to make certain that money flows directly to the GP first in your entity, not the practice.
With a proposed new simplified practice incentive payment set to capture how MyMedicare is mainly incentivised, the program is lining up to work in the opposite way.
It might be that a cleverly worded tenant doctor contract can get around the problem. But it will be hard and messy if it can be done at all.
It certainly isn’t a clear signal of engagement in MyMedicare for most GPs who are operating in a tenant/landlord type administrative set-up, which is most GPs across the country.
For GPs operating as tenants, the call from their administration entity (landlord) to get patients enrolled might end up being seen as more red tape for little direct potential return on their income.
HealthAndLife advisory principal and payroll tax commentator David Dahm told TMR after reading the Incentive Reforms Review that the proposed changes did not seem to be contemplating payroll tax problems appropriately.
“To properly account for the payroll tax ecosystem the Department of Health and Aged Care is going to need to treat individual tenant doctors like they may have thought of practices in the past,” he said.
“That is, each tenant doctor is their own practice, if you want to be clean on payroll tax. To do that they are going to have to seriously contemplate going from PIP and WIP to DIP (doctor incentive payment), which is not what the Incentives Review is recommending.”
Another problem for the DoHAC now: where once the RACGP was tenuously on board with the MyMedicare tighter longitudinal GP-patient relationship concept, now the powerful GP group is lining up against the idea, even if indirectly, because their view of the recent incentive review reforms is that they look like capitation payments.
They hate the idea of capitation payments as a way of remunerating their membership going forward.
RACGP President Dr Nicole Higgins said the proposed PIP and WIP changes articulated “a pathway towards what sounds like capitation – the RACGP will never support this”.
No clear value proposition for patients either yet
So, with individual GPs not really in the picture engagement-wise and the main GP college no longer onside, what about the patient, our other key stakeholder here?
Hmmmm. The expert panel at the webinar admitted that there wasn’t much in MyMedicare at this stage for patients to get excited about. But don’t fret, the expert panel thinks it’s a work in progress and it will work in the end.
One webinar audience member asked the expert panel to expand on the proposed link between incentives and voluntary enrolment system MyMedicare – specifically whether the Department was concerned about patients not seeing any advantage in enrolling.
“I think that over time, we’ve got to use these changes to build continuity of care so that patients understand why it’s good to go and see the same practice and practice team – because the data is quite clear that, when they do, they get way better outcomes,” came the reply from the panel.
“But at the moment, there’s no real mechanisms or link to make that happen.”
Ouch. That’s quite an admission.
If the program is voluntary and there isn’t much in the way of incentives for patients to get engaged properly, how are they going to get engaged again?
“Over time, as we increasingly link these things to a patient who we know, who we’ve got data on, at a practice that we can fund to do needs-based care with the team that will best support that needs-based care, we’re going to get better outcomes.”
In other words, magic will happen.
More of that optimistic, forward planning, just push ahead stuff.
It has the ring of a tactic used by some start-ups termed “fake it till you make it”.
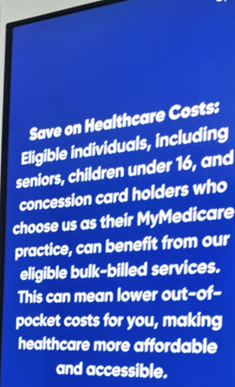
On the subject of actual patient perspective, I was sitting in my co-located pathology room of my local GP practice just last week looking directly at the practice screen and what I got was a pitch from the practice for me to sign up to MyMedicare.
I’m clearly a biased reviewer for this sort of thing because I have a lot more inside dope on what is actually going on than your average patient, but I tried to put myself in the shoes of an average patient and my two key emotions watching the pitch were first confusion, and then, boredom.
Not exactly the emotions that the DoHAC might be going for in patient terms to get this thing rolling well, but immediately recognisable emotions we’ve seen before from patients interacting with other big government-led healthcare transformation projects that have failed due to lack of patient interest – like My Health Record and Health Care Homes.
Even though I know what is on offer for a patient in MyMedicare I don’t think your average patient is going to work it out and if they do they aren’t going to see enough value to get excited enough to ask to join.
There was another problem with my practice screen promotion.
I got pitched four different reasons to join up to MyMedicare as if I got all those things if I joined up. But I know that each thing was for a different type of patient. For example, one was for an aged care resident – and I’m not sure how they would ever see this promo, by the way.
So, my local GP practice feels like it’s being just a bit misleading in trying to get me to voluntarily join up.
I wondered whether that was accidental or deliberate.
Given the practice payments in the offing already per patient enrolled and the promise of so much more to come from the government if you get a lot of your patients joined up, I’m thinking it was perhaps a subconscious mistake.
No matter, I think this could end up as a big problem if things don’t get clearer quickly.
Money is already skewing the motivation of one set of stakeholders (practices), and the acuity of information that the second key other stakeholders – patients – are receiving about the reasons for the program is already getting warped.
Trends like this can obviously lead to disappointed and disgruntled stakeholders.
If at any point patients think we are somehow duping them with MyMedicare, it will fail almost certainly over time.
On that front we asked the DoHAC just how many patients had so far enrolled in MyMedicare and they told us its 1.5 million. Their target for the program once it’s properly bedded in is 11.5 million patients.
We aren’t sure what to make of that number after one year, but maybe the DoHAC has planned for a gradual start.
Related
The digital infrastructure to manage the program isn’t in place
Another problem: the panel is saying that although we don’t have great hooks for patients to get engaged yet, over time the data we collect and process will inform better care and the patient will eventually see that advantage.
What data though, captured by who and in what way?
Already we have seen significant issues with the major software vendors struggling to build out the functionality required just for enrolment in MyMedicare.
Talking to one of the two major GP patient management system vendors this week about the problem they commented that they aren’t being funded nearly enough to build the sort of functionality that people on the incentives panel were talking about for data capture and analysis.
Which begs the question. Even if we do manage to enrol enough patients of the right demographic over time, will the appropriate digital infrastructure be in place to manage the aspirations of the policymakers in terms of far more finely tuned data collection and analysis, so the government can fund MyMedicare appropriately for its outcomes?
Build it and they will come
A lot of what is going on in terms of how MyMedicare is being rolled out at the moment has an air of “build it and they will come” (maybe look up “cargo cult”).
That was a fundamental problem with the My Health Record project.
So far the key patient management software vendors aren’t sure of what they need to build and they are very worried that they aren’t going to be funded to build it properly anyway.
While MyMedicare is proposing to pay doctors and practices to build out the program, and intends to offer patients much better care as an attraction, there is no obvious immediate additional revenue or profit for the major PMS vendors in building out the new data capture and sharing functionality that MyMedicare looks like it is going to need.
We are focusing on the aspiration and the idea without having quite a few of the foundational building blocks for success in place.
We’ve had an interesting policy idea, we’re starting to execute it, we are changing it as we go, we aren’t going to trial or test it properly, but we are saying that the two major stakeholders, who we haven’t involved really in the design that well – doctors and patients – are somehow going to see how good our idea is and start engaging and participating enmasse.
We are also assuming the software vendors will build new functionality without any real incentive for them to build it.
Is it voluntary or mandatory?
Not far into the Incentives Review paper you will see two recommendations which are pretty surprising and I guess are the fallback for the DoHAC if we don’t suddenly get that engagement from doctors and patients the incentives review panel seems to think we are going to get.
- require general practices and patients to participate in MyMedicare.
- require general practices to provide comprehensive service delivery information, and data to support calculation of reimbursements, planning, evaluation, monitoring of health outcomes and quality improvement.
A fundamental tenet of MyMedicare to start with was that it was a voluntary program.
According to the review consultation paper, it’s going to shift to mandatory if you want to get the incentives.
That’s about as big a U-turn as the decision the government made to switch the My Health Record to “opt out”, when nobody was opting in on a voluntary basis. What it meant was everyone was automatically opted in to the My Health Record, if they did not actively opt out.
Forcing engagement on anyone rarely works.
When the government went to opt out on the My Health Record it did not stop to consider the fundamental problem they had – that the product wasn’t good enough (useful enough) for either providers or patients to start using it.
The government then simply tried to force it.They doubled down on investment and shifted the whole system to near-mandatory participation. What they got was a whole lot of people who were now joined to the project who still didn’t participate in it.
The My Health Record still isn’t useful enough and accessible enough in a system context for people to want to engage with it enmasse.
The other problem the My Health Record had, which feels eerily similar to where MyMedicare is heading, is that the base digital infrastructure surrounding the project was not in place for it to ever work the way it was envisaged by the policymakers.
MyMedicare feels like it is in imminent danger of repeating the same mistakes as the My Health Record.
The most fundamental mistake so far is assuming it’s such a great idea that the key stakeholders will take to it like ducks to water (if patients and doctors are ducks in this metaphor, then so far we’re missing the water).
That didn’t happen with the MyHealth Record and Health Care Homes because the product design did not contemplate properly how to get the patients and doctors interested and engaged – or, to put it bluntly, each program did not provide any additional utility to the daily lives of doctors and patients to get them using each program.
When MyMedicare was conceived within the Medicare Taskforce, the authors said this about the concept:
“[It] needs to be supported with a clear and simple value proposition for both the consumer and their general practice or other primary care provider. Participation for patients and practices needs to be simple, streamlined and efficient.”
Where is the simple value proposition?
The second big mistake is that we don’t really have the digital infrastructure in place to do what the policymakers want the program to do – generate, collect and analyse great longitudinal patient data that can be used over time to optimise care.
In this respect we don’t appear to have contemplated incentivising the major software platform vendors in a manner that will get that infrastructure in place to align with where the program wants to go.
MyMedicare is not bad idea.
Its baseline concepts make complete sense for a system that needs desperately to transition to managing chronic care in the community in a much more efficient manner.
But we have a lot of red flags now around its initial execution and near-term plans for further rollout.
Rather than rushing in and winging it with the excuse that we have no time to wait in GP Land for more or different types of funding, as the GP Incentives panel suggested to its audience last week, the government needs to pause for a bit to look carefully at some of these obvious emerging problems, and look at them in the light of past mistakes made on big health transformation projects like the My Health Record.
At this point of time, MyMedicare has a lot in common with when the My Health Record went well and truly off the rails, and we wasted a large part of $2 billion.





