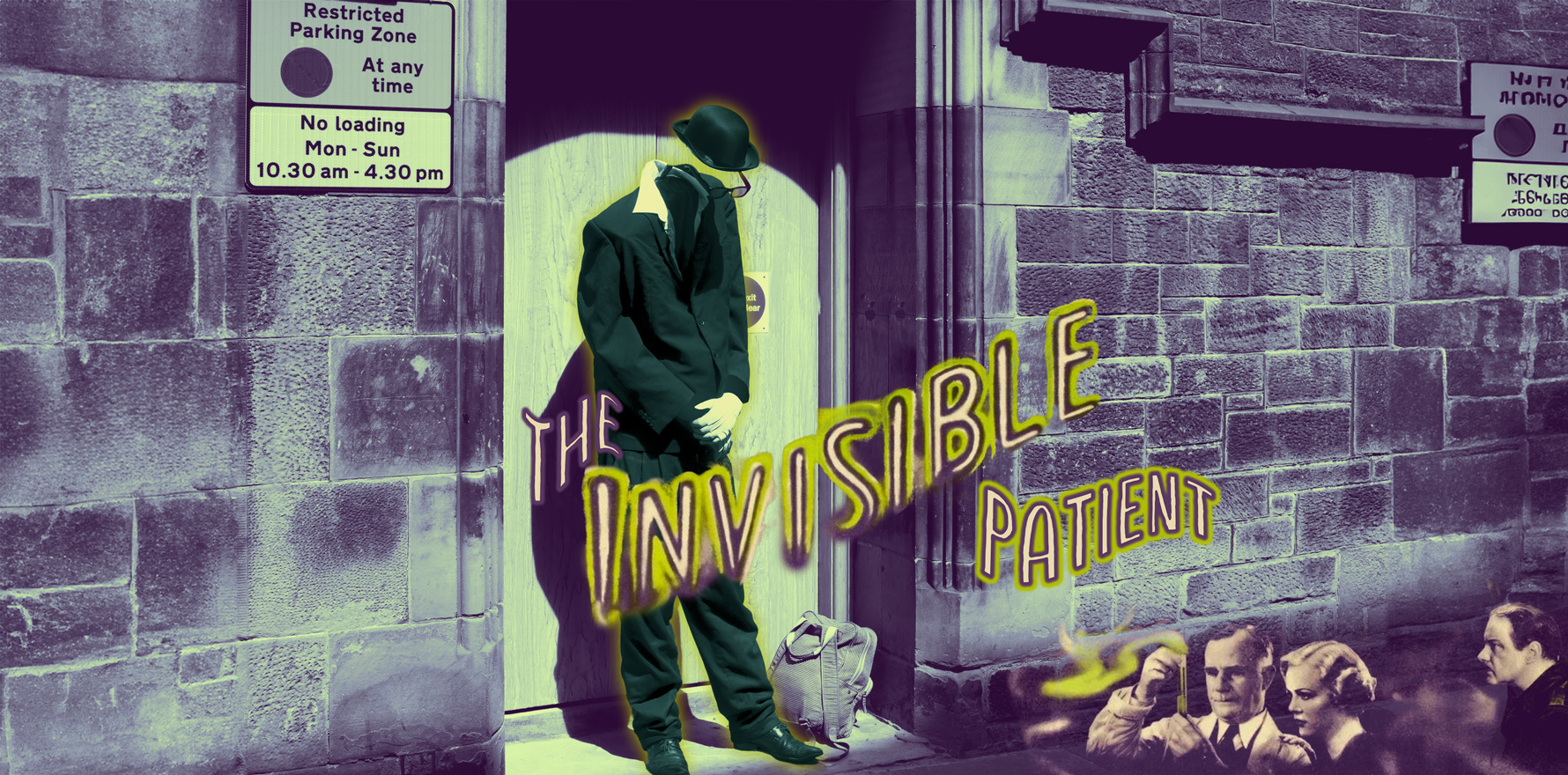
Policy makers are blind to the majority of mental health patients who do not fit a neat procedural model.
There has been recent discussion about the light involvement of GPs within the federal Mental Health Reform Advisory Committee.
The committee has been established to “consider mental health reforms from a whole-of-system perspective” which “includes findings from the evaluation of the Better Access initiative and the broader evidence base”.
Better Access is a program based on a procedural model of mental illness and treatment. The idea is that mild to moderate mental illness is best managed with a diagnosis of a disorder, the implementation of brief evidence-based therapy, and the measurement of an outcome using a standardised tool. It is a model that is grounded in physical illnesses: diagnose cataract, implement evidence-based lens replacement and measure improvement in vision or diagnose hip fracture, do a hip replacement and measure the ability to walk.
It is an attractive model, with easy metrics and some evidence for mild-to-moderate first-episode single-disorder management in depression and anxiety.
However, mental illness is broader than cataracts, mental health care is not as straightforward as hip replacement and measuring mental health outcomes is challenging.
Mild-to-moderate first-episode single-disorder management covers a small proportion of the patients that need mental health care. One author points out that up to 85% of his patients with depression do not fit within the population studied in clinical trials. I would agree. When around 65% of people with depression have mental health comorbidities, and over 50 % have physical comorbidities, applying evidence from first-episode single-diagnosis data to the whole population seems a little optimistic.
In itself, there is nothing wrong with providing care for a small proportion of the population needing mental health management. The problem is we aren’t managing the patients who fall outside of this narrow definition of mental disorder.
If this committee is to look at the entire mental health care system, it needs to understand the people who are currently excluded from it. At the moment, most are cared for in general practice. Unfortunately, the chronic underfunding of general practice has meant the most affordable and effective part of the health system is dying. The implications of policy decisions to underfund general practice is that there are large groups of people with deep mental health needs who are missing out on care and are invisible to the policy makers in this space.
Who’s missing out?
1. Poor, marginalised and isolated patients
We know that the poorest fifth of the population have three times more mental illness, but receive a third of the care. They cannot afford Better Access services and are more likely to have complex needs excluding them from state services. Although they have the illusion of access to online resources, they may not have the literacy, health literacy or devices to use them.
2. People with complex mental health needs
GPs do not treat disorders, we treat patients. This means our understanding of mental illness stretches beyond disorder management. We treat depression in people presenting with inflammatory bowel disease, iron deficiency, heart disease and chronic pain. We treat inflammatory bowel disease, iron deficiency, heart disease and chronic pain in people presenting with depression.
Some of our patients are “pre-contemplators”, where our job is to slowly introduce the idea of mental illness so they can begin to consider treatment. Others present with conditions that are not disorders at all, but still need mental health care. Patients with grief, domestic violence, substance abuse, sexual assault and carer stress deserve as much care as the patient with a DSM diagnosis.
Similarly, there are patients who don’t “fit” the Better Access model, including patients in nursing homes, patients with long-standing sequelae of childhood trauma, and others who are coping with discrimination, marginalisation and ongoing abuse. Patients needing palliative care, parents of children with disabilities, survivors of birth trauma, people coping with chronic pain and others who simply live with constant, unfixable psychosocial suffering seek support in our consulting rooms. They may not have “disorders”, but they do have needs, and they have a right to care.
What do we need to provide appropriate care?
1. Appropriate evidence
General practice continues to see the patients who do not fit, cannot access or don’t benefit from other state or federal mental health services. By definition, this means the evidence generated for standardised patients is unlikely to benefit many GP patients.
Yet the one piece of evidence we had to understand mental health activity in general practice has been defunded. Without BEACH, policy makers have no idea what GPs actually do. Instead, we are stuck with counting mental health item numbers, a poor metric that massively underestimates mental health activity.
Experts like Stephen Duckett and Ian Hickie, both of whom are key members of the Mental Health Reform Advisory Committee, are keen proponents of “evidence-based” mental health care, and outcome-driven funding. It’s interesting that outcomes-based funding is proposed as a solution in primary care, but is not implemented in tertiary services where the evidence for diagnosis, management and measurement of outcome is more straightforward (like cataract surgery and hip replacements).
There is nothing wrong with the idea of outcome-based funding in principle, but in general practice, it means defining metrics for the patients living with the greatest uncertainty. The most needy patients who live with greater complexity and multimorbidity are the least likely to fit within any evidence base. Therefore, defining an outcome is always going to be deeply challenging.
As a GP I have a few options, if outcome-based funding is implemented. I can echo other services, and only accept the care of patients who fit authorised models of care to maximise my income. Or I can live with “underperforming” on metrics that bear no relationship to the patients I see.
If we don’t understand the patients and their needs in general practice, how can we possibly decide to apply metrics developed in other settings to measure its value?
2. Appropriate funding
We do the majority of the mental health work in this country for a fraction of the cost of the institutes, the state health services and private psychiatrists and psychologists. We see the most unwell, vulnerable, and marginalised people in the system. We are paid $50 per hour, take home before tax, for seeing them, which is deeply unsustainable and is one of the many reasons why we are losing our best and brightest from the profession.
It is easy to create a show piece in mental health. It makes us all feel better to see a successful health service for a segment of the population. However, if we are committed to health for all Australians we need to measure and support the patients who are excluded from these services. Value-based healthcare initiatives only work if the savings achieved are invested in the patients who aren’t included in the segment of interest: the poor, the multimorbid, the disadvantaged, the rural and remote, the diverse and often the women.
3. Appropriate respect
General practice is currently living with deep disciplinary disrespect. We are cast as “reluctant” to use “evidence-based” technological solutions, when we know the evidence is scanty, the dropout rate for the trials is high, the patients choose not to use the solutions, and the populations who ground the evidence are not from the same populations we serve.
In contrast, there is deep evidence for kindness and an empathic and effective therapeutic relationship that is never cited. Despite the fact that there is more evidence for the quality of the therapeutic relationship than any specific technique or technological solution, we are constantly criticised for not providing evidence-based, standardised, technology-mediated care.
It is a travesty when I look after the most vulnerable patients in the health system, but I cannot support their application for a Disability Support Pension. Apparently, although GPs are cast as the “cornerstone” of the mental health system and do the majority of the mental health work in the country, they are not considered qualified to make a mental health diagnosis on Centrelink paperwork. Instead, my diagnosis needs to “validated” by a psychologist the patient can’t afford.
These attempts to undermine our skills and capacities are simply about demand management, bathed in the rhetoric of “best practice care”, “stewardship” and “patient centredness”. They impede the care we are able to provide our patients, and place both the GP and the patient in a double bind: we are the only people who the patient can afford, but we are unable to care for them due to administrative requirements we cannot meet.
4. True reform
If we are serious about reform, we need to have some serious truth-telling. It is easier to optimise care for the patients already accepted into other systems than general practice, and to hide the outliers, the marginalised, the poor, the isolated, the unfixable and the complex in a system no-one chooses to examine in any depth. It is even easier to reduce the funding available for general practice, and blame GPs for causing the mental health crisis through their lack of motivation, compassion, ethics or skill. It’s just not honest.
At the moment, there is a convenient gap in our understanding of the mental health needs of our community. Unless the Mental Health Reform Advisory Committee honestly and openly engages with general practice, there will be a large piece of the mental health puzzle missing in their analysis and response. I worry that yet again we will be seen as “glorified referrers” in need of education rather than the experts we actually are.
What matters to me is my patients. They are not seen, counted, considered or valued in this debate because they are invisible to policy makers.
Imagine the benefit to system reform if the GP experts providing 50% of the mental health services for 20% of the total cost to Medicare were well represented. Given this 50% only includes services provided using mental health specific item numbers, and our engagement is far higher, one wonders why we only have one seat at the 15-seat table. There must be an underlying reason why the opinions of the people who provide the most efficient mental health services with such high patient satisfaction are unwelcome at the policy table.
The economists, psychiatrists, psychiatrists and managers on the Mental Health Reform Advisory Committee are not the experts in patients they do not count and refuse to see.