As 4700 practices get their onboarding packs, a start date and dose allocation, nearly 70% aren’t sure they can do the job properly and without losing money.
On Friday this week most GP practices around the country received a letter from the Department of Health confirming their invitation to participate in phase 1b of the vaccine roll out, their proposed starting date, and the amount of doses they will be receiving on a weekly basis, for now.
The letter and the accompanying onboarding pack are as logical, detailed and practical as they can be. If you haven’t seen the letter but are interested in looking at one, HERE is one example to look at.
A copy of the Primary Care Provider Onboarding pack can be read HERE.
The DoH explains that because vaccine stock will be limited in the early stages of 1b, start dates and allocations will be dependent on vaccine availability. That’s probably a sensible warning given what has happened to this week’s 250,000 doses due from AstraZeneca in Europe which got stopped by the Italian government which cited greater need than Australia for the stock.
On Tuesday this week Healthed, which runs a fortnightly clinical webinar series attended regularly by up to 1000 GPs (their next webinar is all about the AZ Vaccine), ran one of their Pulse surveys on the issues surrounding the upcoming GP vaccination program. Healthed’s sample (297), demographic spread of GPs and methodology, are representative of the broader GP population with a statistical margin for error of about 6% at a 95% confidence interval.
The key results are summarised below.
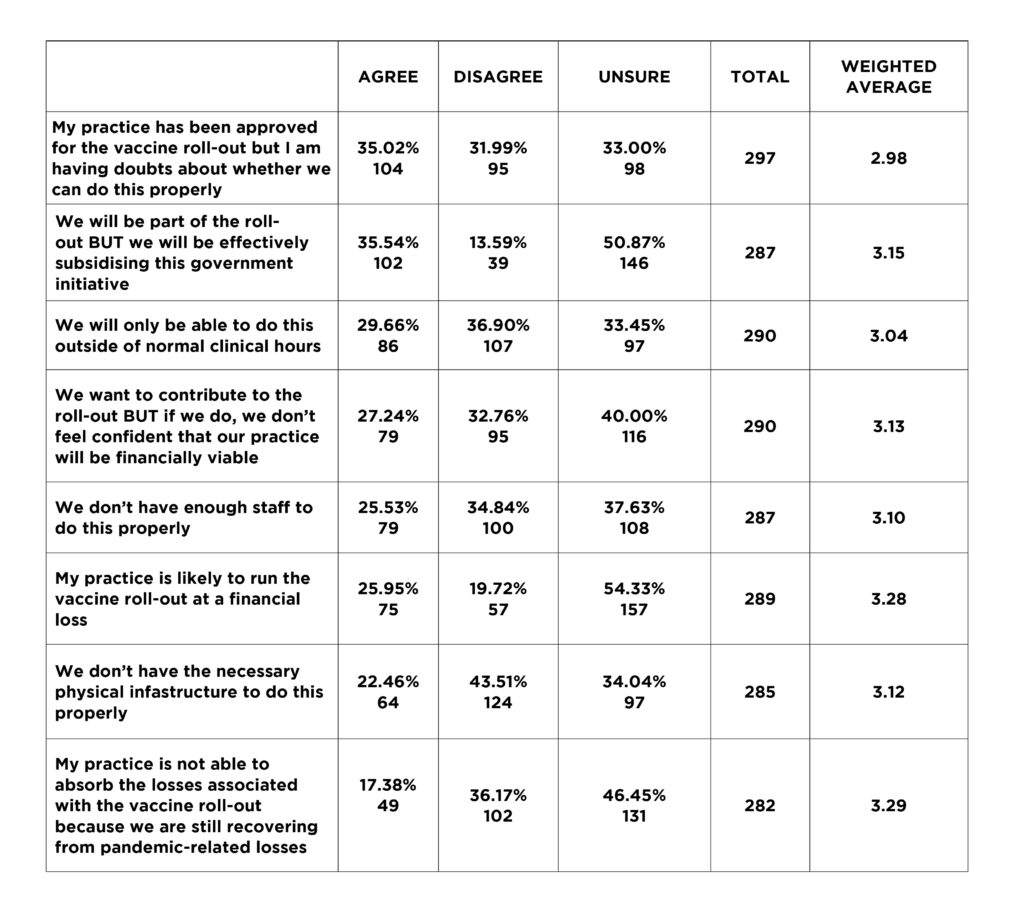
Sixty seven percent of respondents have some form of reservation over their practice’s ability to vaccinate properly, 27% think they will lose money doing it, 40% aren’t sure if they will lose money or not, 22% don’t think they have the necessary infrastructure yet and 26% aren’t sure if they have the enough staff to do the job properly.
The least you might say about this survey result is that prior to getting their starting letter and onboarding packs it looked like there was a significant degree of uncertainty and angst among GPs about their upcoming plans to vaccinate.
Now they all have the starting pack, it seems unlikely the angst and uncertainty will be eased in any way.
This isn’t because the government isn’t trying hard enough, or doing a decent job. Given the set up they’ve settled on, which is distributing to 4700 practices, not 1200 as initially planned, and starting distribution at least month before it has enough stock to meet demand, they are being agile and smart.
The onboarding pack is very detailed, clear on most elements of the rollout, including the timetable and likely supply levels, and covers a lot of the practical issues a practice is likely to encounter.
But unfortunately, in the short term at least, this isn’t going to help much. In fact, some of the new detail, while from a safety view point is likely spot on, from a practice viewpoint will almost certainly add to the uncertainty and anguish expressed in the survey.
An example: pages 11 through 14 of the Onboarding Pack provides important and relevant detail on eligibility and clinical considerations. Proof of eligibility for patients who don’t have proof is going to be one occasional hiccup. In this case, a patient needs to complete a Phase 1b declaration form, a form which isn’t available yet on the DoH website, but we are assured it will be in time.
How complex is that form, and who is responsible to get it and fill it out in the case of some patients who aren’t going to be capable of managing this process?
Just a quick note here on my mum (87), who recently had her pension cancelled by CentreLink because she hadn’t managed to provide the 10 or so detailed financial documents to them on time about her overly complex SMSF. This occurred because her accountant of 30 years was dying of cancer and had managed to forward all relevant documentation to a new account, bar one really important one.
She ended up with no pension, no pension card, no driver’s licence, no passport and no birth certificate.
After a couple of weeks working hard at getting her a whole new pension going, the final hurdle was proof of identity. She had already been on the pension for 22 years, but Centrelink wouldn’t accept that proved she was a real person, even when I got her to appear live before our case officer with a family photo album. We had to go and get a whole new set of proof of identity documents.
Centrelink assured me that the process was logical from the government’s perspective. Im sure it was.
Now my mum is surely an outlier. But if she’d been able to vaccinate a month ago, she would have arrived at her GP bright eyed and bushy tailed. She likely would have left after quite some time, pretty angry, no fault of the GP or herself, without being vaccinated.
Outlier or not, my guess is my mum, unprepared for this proof of identity step once she got to her GP, might have taken at least a half an hour or more to process before having to leave unvaccinated. If she started to get stubborn and upset, which she can, and dig in, bless her, she almost certainly would have ruined the days of several practice staff.
Im guessing my outlier mum, between her first, second and third visit for vaccination, might have lost a practice at least one to one and half hours, without even trying. And that’s not counting the almost certain long term emotional trauma she is capable of causing unsuspecting and innocent practice staff.
The first three to four weeks of this GP vaccine rollout is going to be very difficult for GPs and patients. As we get closer to the actual event, the wrinkles are bing ironed out, with very little give for general practice unfortunately. The government just leans that little bit more in, and assumes GPs will lean even more with them to bear the project creep, the additional complexity, and the additional risk to their businesses. Which they likely will.
Managing patient behaviour and expectation, when supply is going to be limited, might turn out to be particularly tricky in the first month of vaccination of 1b patients.
An example:
- You are medium-sized practice, with around 1000 patients over 70, and say another 300 under 70 who have a chronic condition
- You have been allocated just 50 doses for your first week of vaccination (note: the minimum order allocation according to the stock management pages of the onboarding pack, and box size, is 100 doses – try to figure that out if your allocation is 50 per week, as most practices are at the moment),
- You won’t be supplied those doses until the third week into the start of the GP program, say April 5
- You have been told, in your starter pack, that you shouldn’t book any vaccinations within 48 hours of your expected next batch of doses, once your first batch runs out.
- You have to order that next batch no later than 14 days prior to you wanting to receive it
What can possibly go wrong here between your practice, its normal day to day patient load, and your patients’ expectations around vaccination from their GP?
Obviously, quite a lot:
- You get rushed by your patients as soon as the program start date is announced publicly (this may or may not happen, it is almost impossible to predict)
- Your first batch gets booked out like a Bruce Springsteen concert (within seconds) and your patients start fretting and sending incoming queries on the next available bookings
- You can’t book your second batch until you know when it’s coming, so you can’t answer any of these queries
- Some of your patients, panicked, start booking wherever they can. They book multiple sites to ensure they get an appointment and a vaccination (there isn’t an indication yet that the centralised booking system is using a unique ID and can share the information to prevent this same issue that occurred with last year’s flu vaccine)
- Some of your patients don’t turn up because they got their vaccination somewhere else and didn’t alert you.
And before you even lay your hands on that first batch of 50 doses? You will need register yourself on the COVID-19 vaccine stock management portal to create your unique account, notify your PHN, register your current external booking systems with the portal so they can talk to the central system (presuming that system will work by then), make sure all your staff are trained on the AZ vaccine, re-check your insurance position once you understand the AZ vaccine terms, and so on and so on.
So far it’s not been made clear in writing if you can vaccinate your staff before you vaccinate your patients.
You can’t really keep blaming the DoH for some of these seemingly important details still not being covered off formally. There is just so much to cover in such a large and complex logistics exercise.
In the case you decide to vaccinate your staff first, which seems sensible, your practice might only have 30 doses left for week one. But you’ve had 300 enquiries already.
The point here is not that the government is stuffing up yet again and hasn’t thought this through. It has thought a lot out. It has consciously decided to go wide in the GP network (4700 practices) rather than narrow (about 1200 practices initially planned). There are many reasons to believe this path is better for patients and GPs especially given we are in a situation where we have the time to vaccinate the population this way.
The point is more that as this process unfolds, and things are adapted, as they must be, the government keeps leaning into the GP network to deal with more and more coal-face issues, and more business risk and brand reputation risk with patients.
In terms of business risk, GPs as a business sector are by default now assuming a lot more risk on behalf of the government. Yet,
- They aren’t indemnified by the government, although the vaccine manufacturers are
- The risk of supply mismatching demand is very high at this point, especially given we still don’t have a working centralised booking system, or proof of concept even of how the commercial booking engines will talk adequately to the government’s central system to co-ordinate supply, and prevent multiple bookings by the one patient
- We have no idea yet how patients are actually going to respond to the starting gun on getting vaccinated, which is causing quite a few practices managers to stay awake at night. Patient expectation on mass is not predictable, no matter how much you spend on an education campaign to the public
- The risk that their expectation is not met is mostly being taken at the practice level at this point, not at the level of the DoH.
The government has said that phase 1b will be largely completed within a few months and it is still sticking to the end of October deadline for most Australians to be vaccinated. This deadline is almost entirely political, but the risk of missing the deadline, is being pushed outwards now to the GP sector.
This isn’t even a likely tactic on the part of the government. It’s just the case that in any large project, its always those that implement who end up having to solve the inevitable coal face execution issues, and suck up the associated unplanned additional costs, not the planners. GPs essentially have a fixed price contract here.
The deadline set by the government is generally thought by most experts to be now unobtainable, and that given we have the virus under control, we should be going slower for safety’s sake and for the sake of GPs’ ability to manage their patients’ expectations and their finances much better. If we go slower we should be transparent to patients to manage their expectations better.
Telling patients we are still trying for late October isn’t helping the process, and GPs are at the butt end of risk on the issues of not meeting this deadline now if things start going wrong.
All this while nearly all expert analysis suggests the government is not paying GP practices adequately to vaccinate.
All this while GP practices know that when they get through the hard work of vaccinating the most difficult and risky demographic to vaccinate – patients who are over 70 and who have chronic conditions – pharmacists will get to participate in the next phase which will be much easier to do, and higher volume and return.
Just saying, DoH.
Just saying RACGP ( because it’s the RACGP which says it is the key advocacy body for GPs, yet there is little sign it is getting in the ear of government about this pattern).
Yes, the government has a very hard job co-ordinating this whole rollout, and the whole situation is a national community crisis where everyone needs to pitch in. Yes, it has done much to co-ordinate this extraordinarily difficult process which has a very high degree of difficulty.
But you can’t simply sit back and keep loading the complexity and risk of the rollout onto the GP sector, especially when you change your mind substantively on how you are doing it at the last minute, without some give, surely?


