One size does not fit all when assessing symptoms in peri and postmenopausal women
Mood disturbances, such as anxiety, depression and psychological distress are more common among women than men, though we still don’t know why.
Results from the Australian Bureau of Statistics’ National Health Survey (2014-2015) reported 11.7% of adults experiencing high or very high levels of psychological distress: 13.5% of women and 9.9% of men. In 2010, Williams et al, reporting on the prevalence of anxiety disorders in Australian women, concluded that one in three women (34.8%) had experienced some form of mood and/or anxiety disorder.
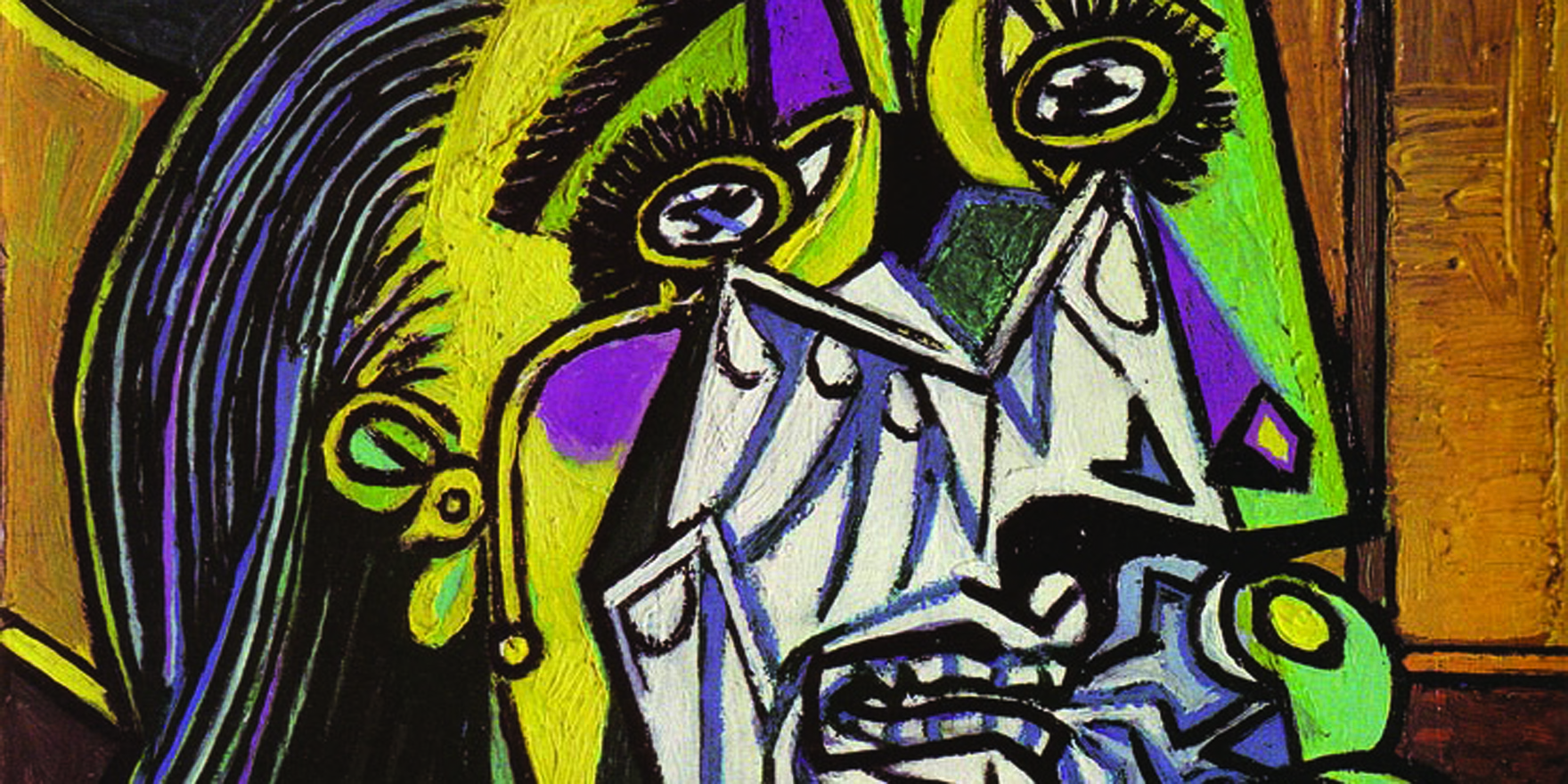
Mood is a complex, multifactorial phenomenon that may include symptoms such as anxiety or feelings of panic, psychological distress, euphoria, tearfulness, persistent depression and irritability.
Mood disturbances occurring during periods of hormonal fluctuation, such as the postpartum and premenstrual periods and the menopausal transition, have spawned many theories regarding hormonal influences on mood.
However, while hormonal explanations for postpartum depression and premenstrual dysphoric disorder are well documented, no such causal relationship has been established for the menopausal transition.
Indeed, some of the alleged symptoms of menopause can often be attributed to factors other than changing hormonal levels: even the classic hot flushes, night sweats, and disturbed patterns of sleep are not always purely menopause-related.
Personal stress, changes in the quality of a relationship with a partner, and other psychosocial and lifestyle factors can all significantly affect mood during the menopausal transition, since that phase of a woman’s life – often associated with major life changes such as “empty-nest” syndrome or death of a parent – can be challenging. For some women, the mere onset of menopause can be a challenge to the sense of identity and value, even in the absence of any hormonal influences.
Cross-sectional studies consistently show the highest prevalence of depression occurs in women during the reproductive years, whereas longitudinal studies of women during the menopausal transition have been contradictory. Very often it appears that age itself, rather than menopause is the primary influence. For example, the prevalence of sleep disturbances increases significantly in middle-aged women, but there is no proven connection between sleep disorder and hormonal changes.
While the US Study of Women’s Health Across the Nation showed correlations between poor sleep, hot flushes, anxiety, depressive symptoms and lower oestrogen levels, they were not shown to be causal: as with changes in mood, many mid-life factors unrelated to menopause may disrupt normal sleep patterns (for example, work issues, relationship or financial difficulties, or family upheavals).
We simply don’t know whether common symptoms reported by mid-life women going through the menopausal transition are associated with hormonal change, and we also don’t know whether those symptoms derive from a single cause. Recent research has focused on the idea of “subsets of symptoms” that may respond better to treatment such as hormone replacement, designed to address the cluster as a whole rather than individual symptoms.
As usual, one size does not fit all: peri- and postmenopausal women must be assessed and treated as individuals, where their life situation is likely to be just as significant as their hormonal state.
Dr Sheila O’Neill is chair of the local organising committee for the 21st Annual Congress of the Australasian Menopause Society being held at the Sofitel Wentworth Sydney 13-15 October 2017.
References:
1. Australian Bureau of Statistics (2015). National Health Survey: First results 2014-2015. Cat. No. 4364.0.55.001. Available form URL:http://www.abs.gov.au (accessed 16 Aug 2017).
2. Bromberger JT, Schott LL, Krabitz HM, Sowers M, Avis NE, Gold EB. (2010) Longitudinal change in reproductive hormones and depressive symptoms across the menopausal transition: Results from the Study of Women’s Health Across the Nation (SWAN). Arch Gen Psychiatry 67:598-607
3. Campbell KE, Dennerstein L. Finch S. Szoeke CE. (2017) Impact of menopausal status on negative mood and depressive symptoms in a longitudinal sample spanning 20 years. Menopause 24(5):490-496
4. Greenblum CA. Rowe MA. Neff DF. Greenblum JS. (2013) Midlife women: Symptoms associated with menopausal transition and early postmenopause and quality of life. Menopause 20:22-27.
5. Vesco KK. Haney EM. Humphrey L. Fu R. Nelson HD. (2007) Influence of menopause on mood: a systematic review of cohort studies. Climacteric 10:448-465.
6. Williams L. Jacka F. Pasco J. Henry M. Dodd S. Nicholson G. Kotowicz M. & Berk M. (2010) The prevalence of mood and anxiety disorders in Australian women. Australasian Psychiatry 10:448-465.