The resumption of world travel, especially the Hajj this week, raises the risk of another, rarer virus.
GPs should be aware that travellers who return from the Middle East unwell may have been exposed to the MERS coronavirus, the Department of Health has warned.
Between 7 and 12 July, millions of Muslims worldwide will make the Hajj, or pilgrimage to Mecca in Saudi Arabia. This is the first time in three years that Australian Muslims have been able to make the journey.
A full travel and exposure history should be taken from patients who present with symptoms, the DoH said, and should apply infection control measures as soon as they suspect Middle East respiratory syndrome. There is no vaccine.
MERS is a notifiable condition, and GPs should contact the relevant state or territory public health unit where there is a suspected, probable or confirmed case. They can then discuss patient testing and referral.
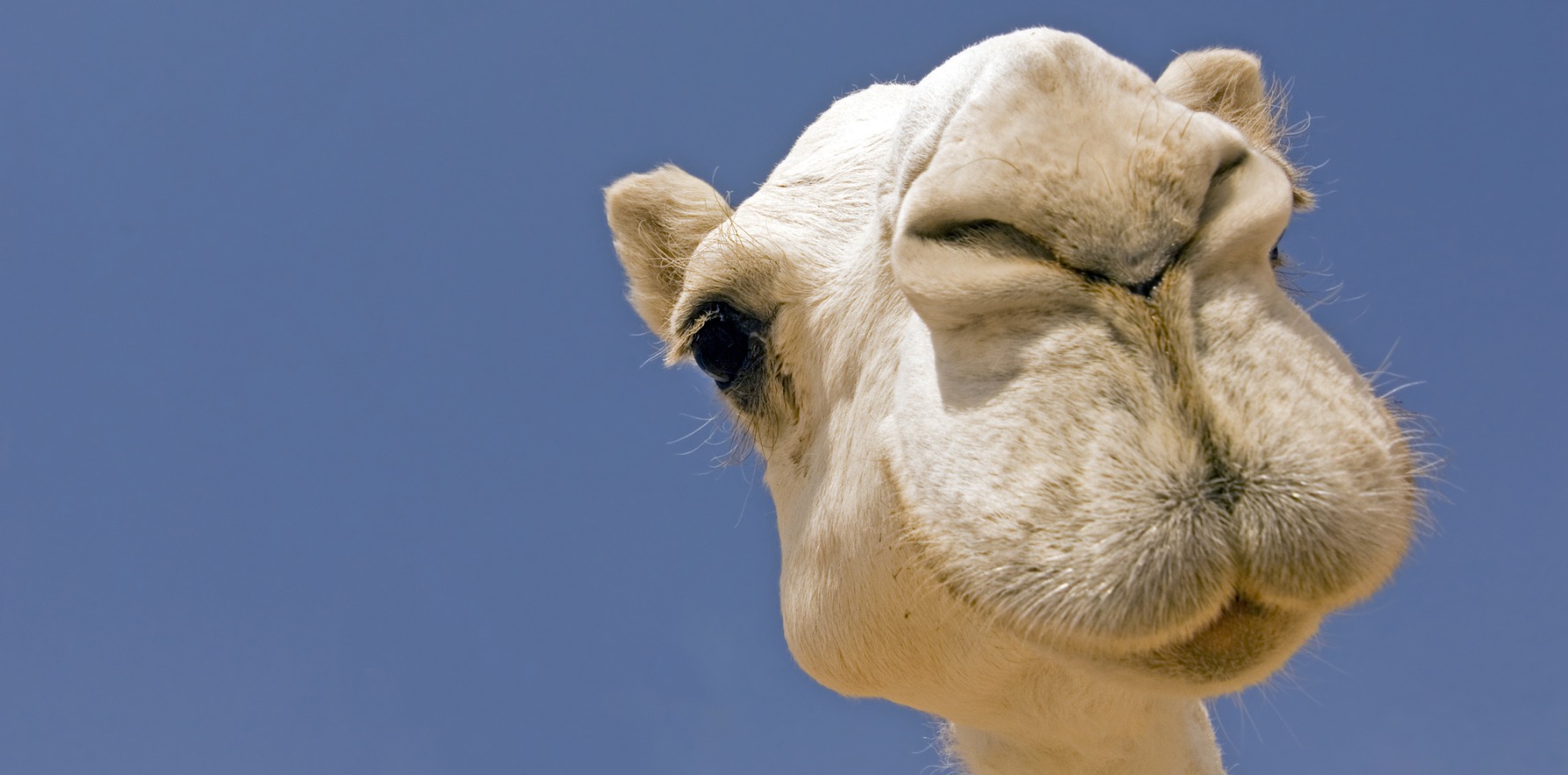
Qatar reported two laboratory-confirmed MERS cases between 22 March and 3 April this year. However, the WHO expects further cases in the Middle East and countries where the virus is circulating in dromedary camels.
Chronic conditions such as diabetes, renal failure, chronic lung disease and immunocompromise put individuals at greater risk of severe disease.
Individuals can be exposed to the MERS virus through contact with dromedaries or their products, including raw camel’s milk, or with another infected person – particularly in healthcare settings. MERS has so far not been demonstrated to transmit from asymptomatic cases to their contacts.
The WHO has recorded 2585 laboratory-confirmed cases and 890 deaths since the first cases were reported in September 2012. All cases have been linked to travel to or residence in Middle Eastern countries.
In patients with compatible symptoms and exposure history, the DoH said GPs should follow standard and transmission-based precautions (contact, droplet and airborne) for infection control, to minimise the risk of spread of MERS.
The RACGP has infection control standards for office-based practice on its website.
MERS is unlikely to be the cause of a pneumonia or pneumonitis case in Australia, but health professionals should investigate as usual, bearing in mind the patient’s travel and exposure history.
Patients who present with fever as well as pneumonia or pneumonitis or acute respiratory distress syndrome should be tested for MERS if they have travelled from or lived in affected countries in the Middle East within 14 days before the onset of symptoms. Other patients might also be eligible for testing based on their exposure history, including those who have had contact with a symptomatic traveller or contact with camels or raw camel products.
The DoH warned GPs not to collect clinical samples in a general practice setting. Patients should be referred to a hospital for investigation and management, ensuring ambulance crews are aware of the reason for the referral.