An awful lot of money is being spent on COVID-19 telehealth – but where is it going?
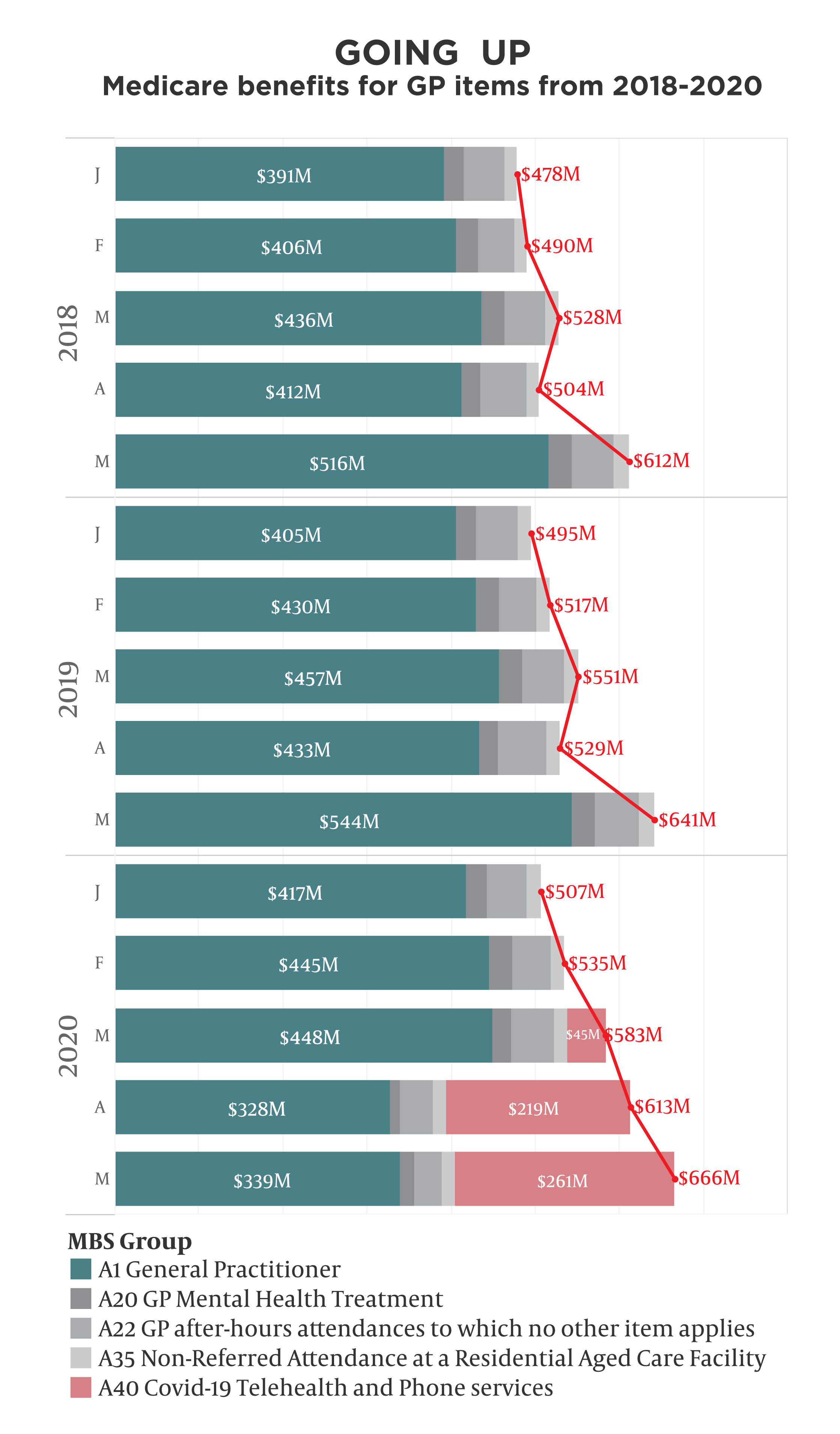
MBS data for May shows that payments for GP items have continued to rise, both month on month and compared with the past two years – thanks to more than half a billion dollars spent on telehealth.
The data shows enthusiastic take-up by patients of rebatable phone and video consultations, which are due to expire on 30 September but are in fact likely to be extended in some form yet to be determined.
An analysis by The Medical Republic of a selection of items in the latest Medicare statistics shows that overall GP billings have gone steadily up since the start of the year, with COVID-19 telehealth payments more than making up the shortfall in regular face-to-face GP attendances.
Billings for all these items totalled $667 million in May, $261 million of which was for telehealth. That’s up from $614 million (and $219 million) in April, and up from $643 million in May 2019.
This data does not, however, show how these payments are distributed across providers.
Anecdotally, GP practices experienced a marked drop in business from patients staying away during the first months of the pandemic.
With many companies already set up for private telehealth before the pandemic, and able to market their remote consultations more effectively than local practices, it is likely they have been able to scoop up a significant proportion of the telehealth consultations while small practices have been playing catch-up.
The RACGP and AMA are both advocating for the continuation of Medicare-rebated telehealth after 30 September, but have expressed concern that “call centre” models are popping up that will skim the easiest consults and leave the harder ones to bricks-and-mortar practices, threatening their viability – especially in the country.
Basic in-person GP visits are still well down from January, which is typically the slowest month of the year – but they are creeping back up after a very large drop-off in April. The $339 million spent in May is almost 40% down on last May.
The data shows that attendances at residential aged care facilities have remained constant, while after-hours attendances have shrunk. Face-to-face mental health attendances are rising again.
Changes to the PIP scheme, in which more payments go to practices rather than individual GPs, explain why that category is down – if that weren’t the case, the overall payments would show an even bigger increase.