Our poll shows the level of stress GPs feel about the PSR bogeyman and how it affects their practice.
I’ll keep this short (lol, and a quick shout out to Stuart and a few other fans of my Saturday ramblings)
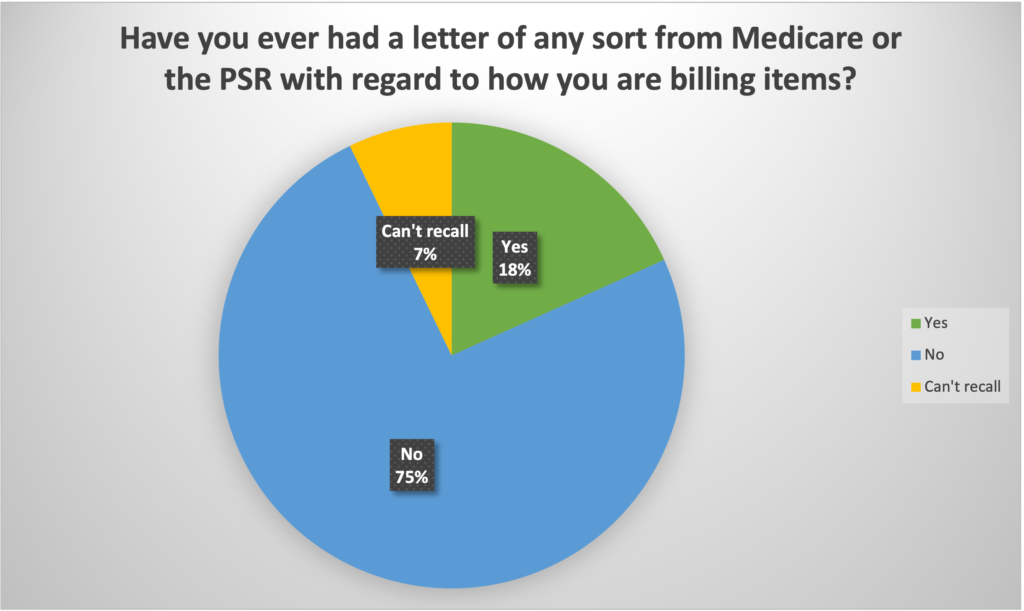
In more than 20 years of being involved in medical media and publishing, I’ve never seen as big and as fast a response to a survey as we had this week on the subject of Medicare audits (the PSR), its effect on the morale and wellbeing of GPs, and how that effect ends up warping the delivery of optimal medicine to the public in this country.
In just two days we’ve had over 1400 responses to our survey, in large part thanks to Healthed’s PULSE survey service, which they conduct now every fortnight when they put on their fortnightly live webinars (which an amazing number of GPs regularly attend – 3,000 last Tuesday, which is another story one day).
But also, simply because GPs are obviously seriously engaged now in this issue.
From a stats point of view, there’s significant confidence in the results.
I could easily blurt out a few thousand partly incomprehensible words here, but I think the results, in the form of the basic results charts for each question, speak largely for themselves.
We provide just a few observations below to get you going, and perhaps interested in looking over all the results a little further.
Also, we don’t want to overly influence what you make of the data. Make your own assessment and we can talk further if you’re interested in deep diving on any aspects of the results so far.
We’ve provided a separate place to send ideas, questions and suggestions if you have any, although feel free to comment below as well.
If you haven’t taken the survey but would like to now, please do so.
We think we are already at a statistical level that will be very hard for the government or other detractors to ignore (hmmm … they are pretty good at ignoring stuff, so perhaps we’ll reserve any call on this for a couple of weeks).
Notwithstanding, the more GPs that take the survey the merrier from here on in, just in case.We are also working with some statisticians and professional researchers this week with a view to delivering a more formal dissection of what the data we have collected means.
There appear to be some very interesting devils hidden in the statistical detail of the data. Feel free on this front to ask us what might be on your mind to understand better (we have detailed demographics to dissect responses) but not clear in the data below.
Some high-level observations to start things rolling:
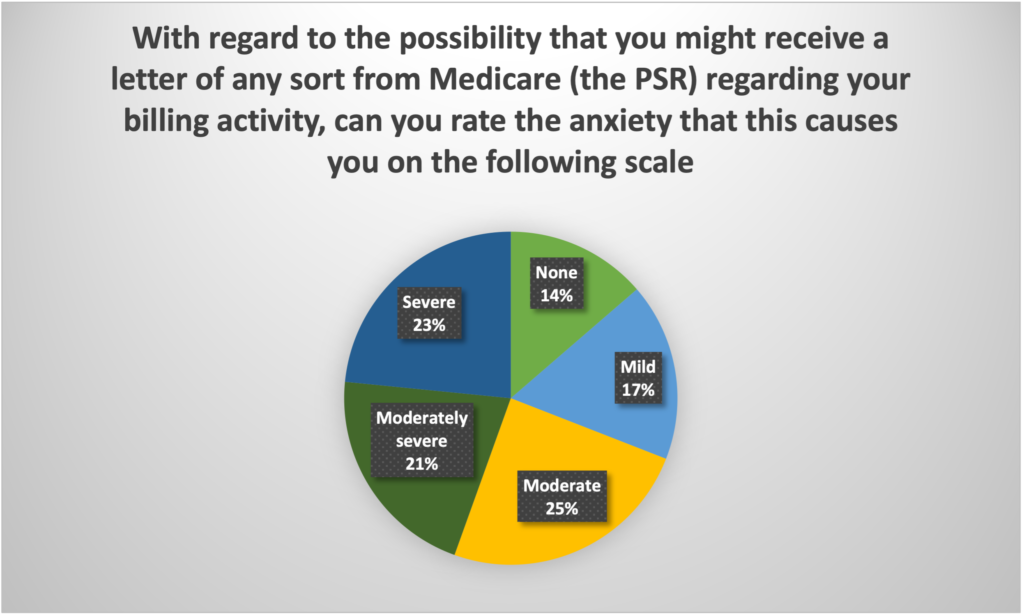
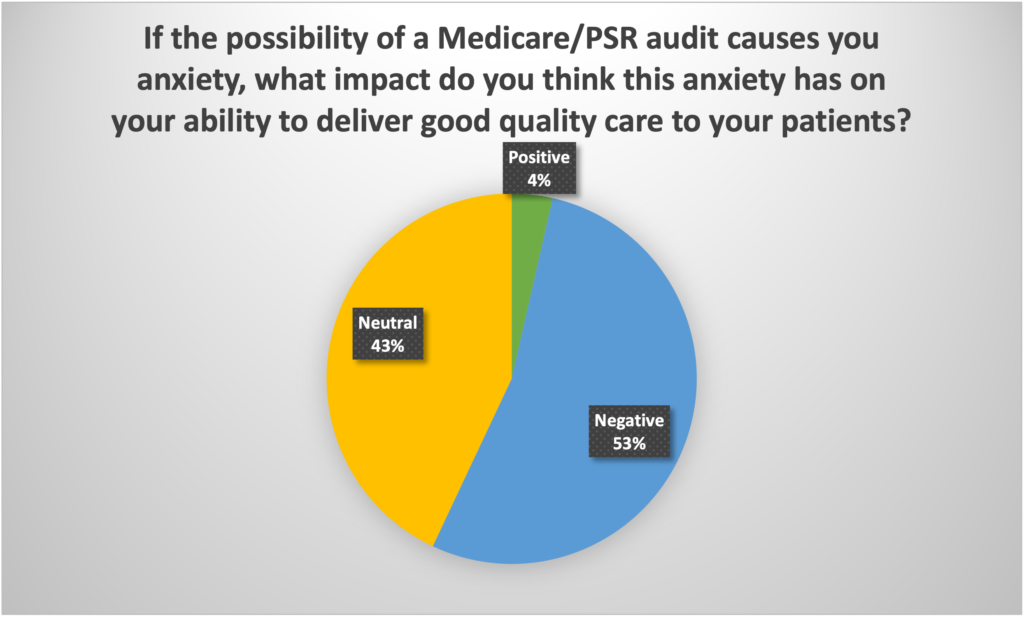
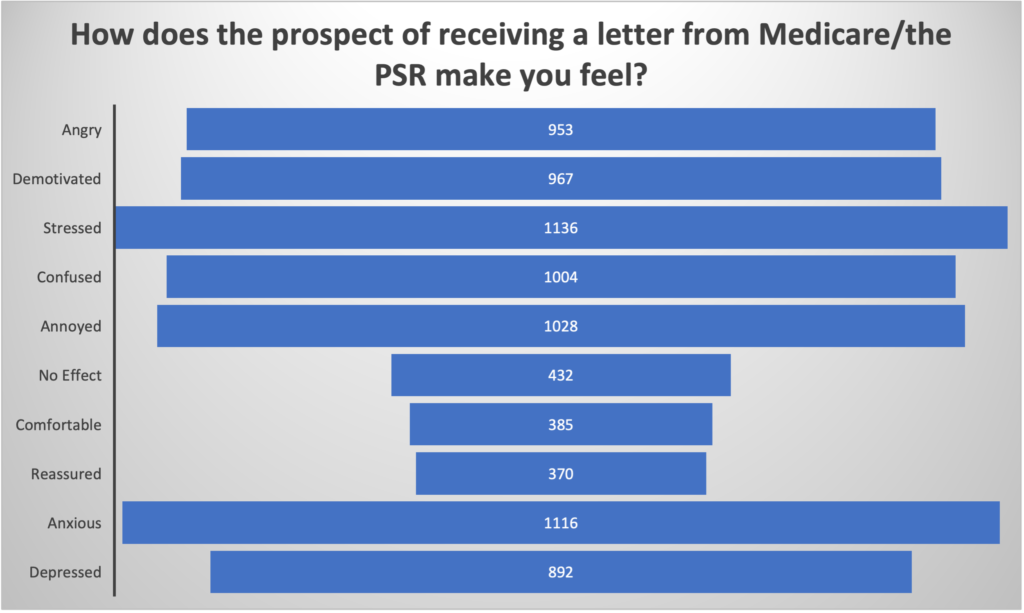
- Almost 70% of GPs feel moderate, moderately severe or severe anxiety with simply the idea that they might one day get an audit letter from Medicare/the PSR.
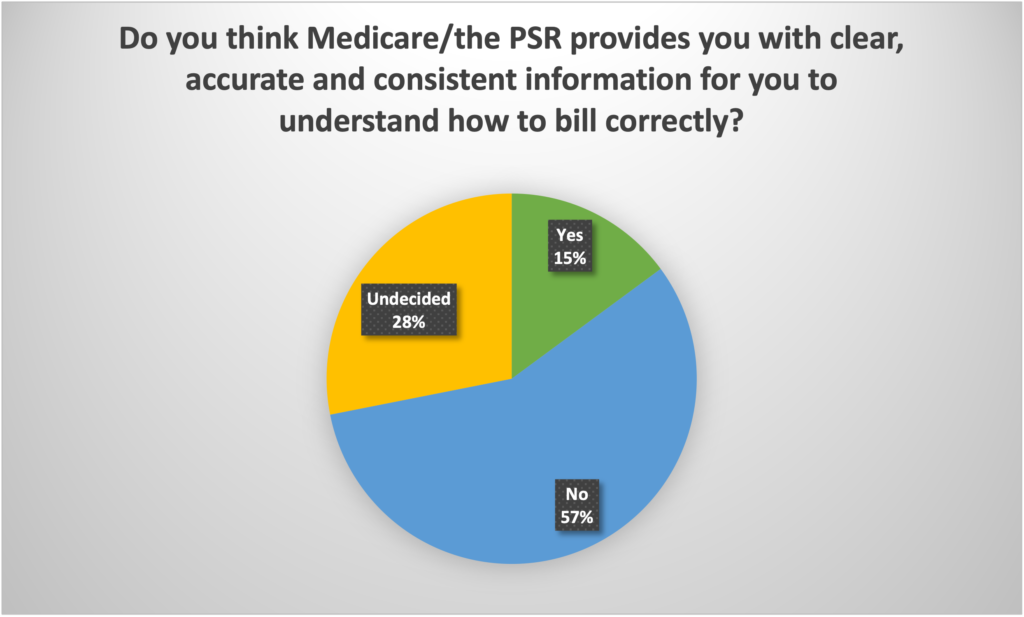
- Nearly 60% of GPs don’t think they are provided with clear, accurate and consistent information to guide their billing practices by Medicare.
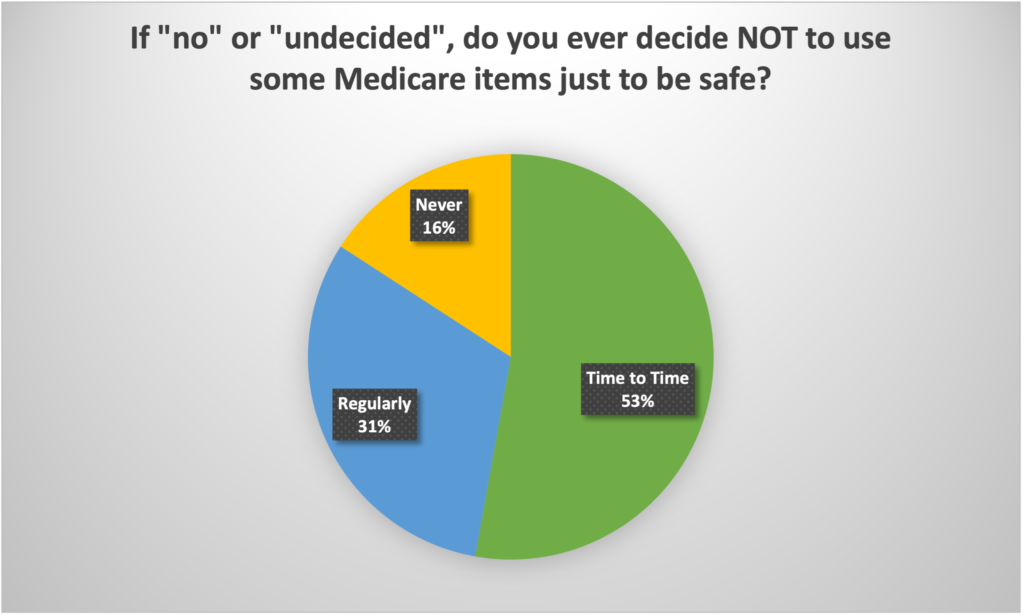
- Over 84% of GPs, regularly, or from time to time, don’t perform certain services because of anxiety over whether the PSR might deem their performing those services to be inappropriate.
In simple terms, the majority of Australia’s most important frontline healthcare professionals live in not insignificant fear of the PSR and a Medicare audit, and alter how they deliver medicine based on that fear.
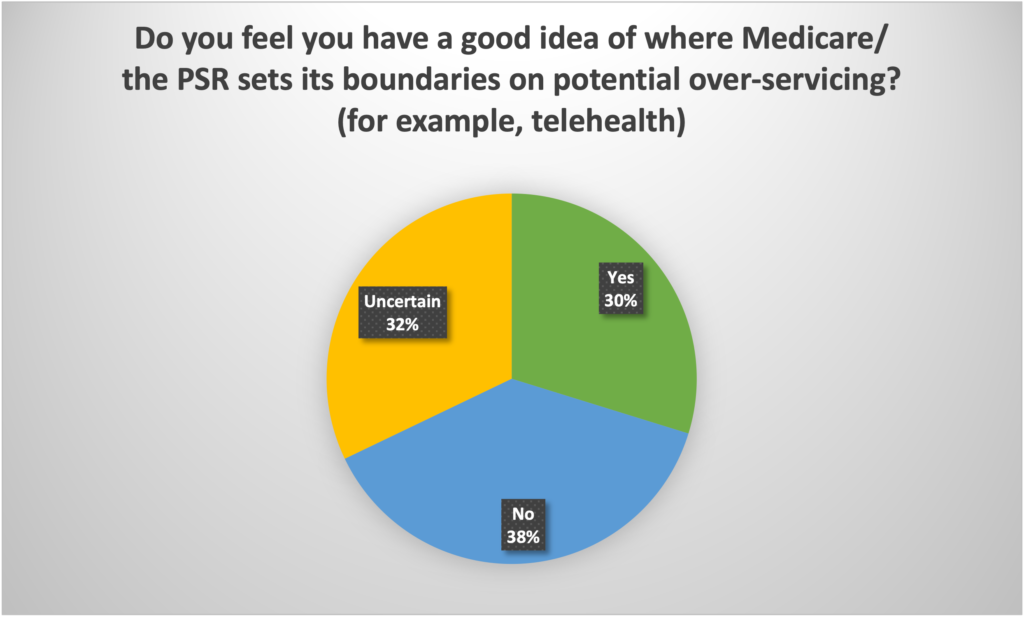
The fear stems from how the PSR conducts itself and because most GPs believe they aren’t being provided with clear and consistent information to make the right judgment on how they bill.
At its bare bones: the most effective delivery of medicine in primary care is being warped, possibly significantly, by a system the government is using to govern its costs in Medicare.
It’s pretty hard to see how this set-up could be in the public interest.
Yet the PSR is embedded in law that we now know is almost wholly stacked against GPs. If the PSR deems you’ve done the wrong thing, you’re toast. Only one doctor has ever won a case against the PSR. That was 20 years ago, it was only a part win, and after that the Department of Health changed the law to close the loopholes by which this doctor emerged partly successful in proceedings.
A few more important observations:
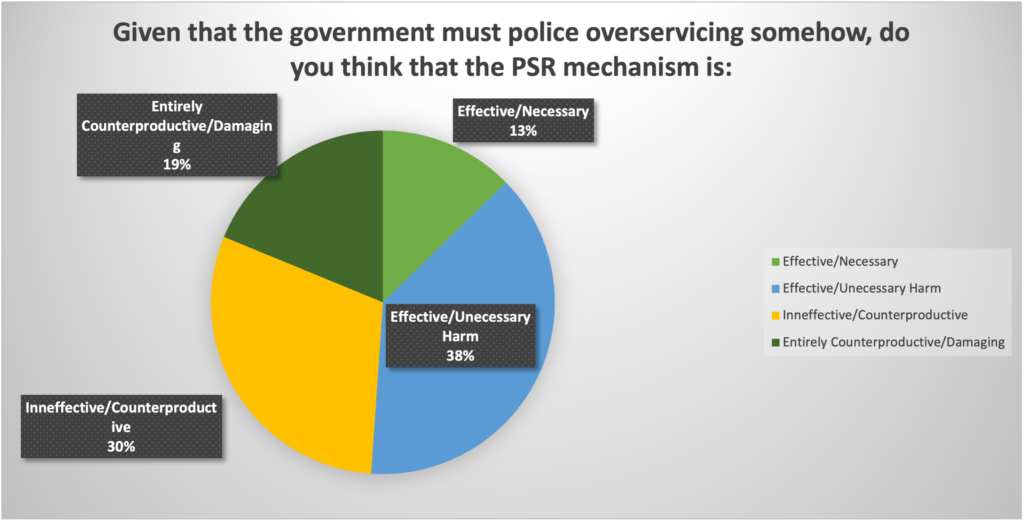
- It’s not as if the government can’t come up with something more transparent, and reasonable. GPs can’t not be monitored while spending so much government money but they can in a much fairer and productive way.
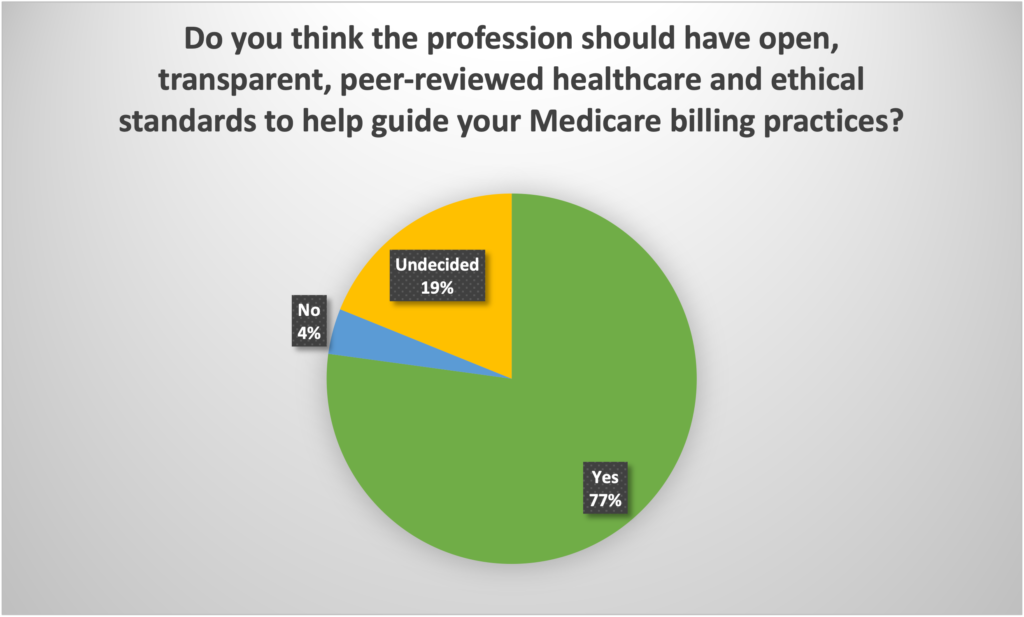
- GPs would love a set of clinical and ethical standards to be guided in how they behave and bill. In fact, 77% of GPs want this sort of mechanism to clear up this problem. Only 4% don’t want it. The colleges and the government could work these standards out, like other professions have.
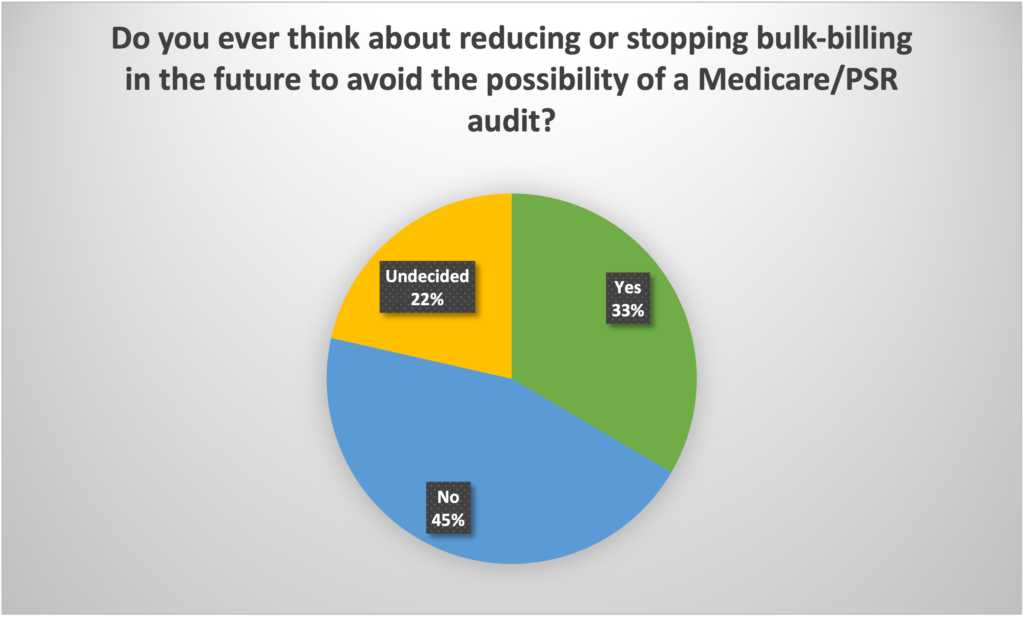
- The whole problem is creaking under pressure in a manner that isn’t good for anyone, even the government trying to keep its budget in check. Nearly 35% of GPs are thinking of giving up or reducing bulk-billing entirely in order to escape this governance regime, so badly do they think of it.
There are lots of other interesting data in the questions that point to the system starting to break down.
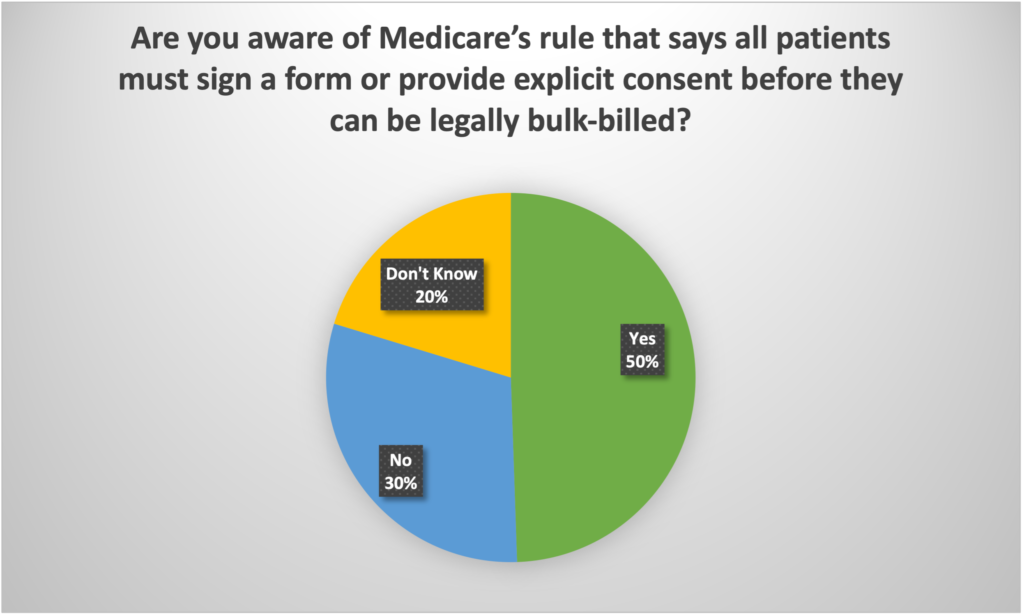
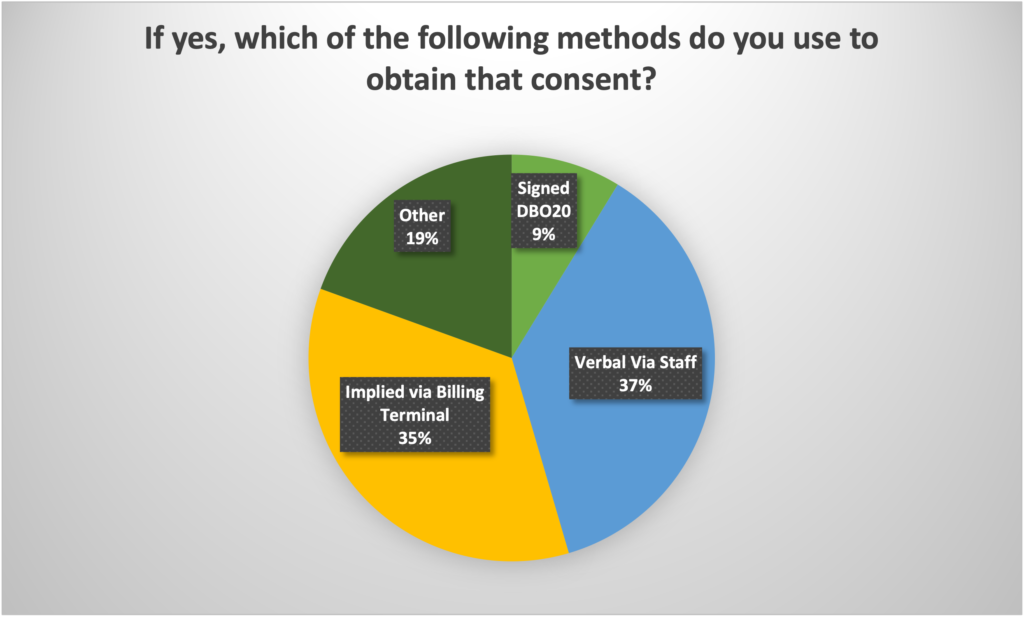
An interesting piece is that most GPs either don’t know that they are required to get proper consent from a patient for each billing item in Medicare, of if they do know, they aren’t doing it in a way that legally the government could ever really enforce if push came to shove and some clever lawyer asked the government to prove that assignment of the rights to bill the Medicare item directly to the doctor was ever actually given.
In just this question there is a potential nest of pain for Medicare executives. Consent is not a practice PA hitting YES on a billing terminal in a court of law no matter how practical that work around seems to be.
There’s a lot in here that just doesn’t add up, is creaking with too much weight of evidence around counter-productivity, and, simply, unfairness.
I’m wondering what happens from here.
It will be interesting to see if the colleges can make something of this data, or if not this data, generate some of their own given that these questions seem to be very close to their constituents’ hearts.
We will be collecting more results and dissecting the total sample in more detail with people who know what they are doing.
It can’t keep going the way it is now – can it?
Survey results (N = 1430)