Data overload and multiplying patient alarms are causing stress and confusion for care teams. In this webinar four experts discuss the problems of digitising a hospital and how to solve the complexity.
The building of digital capability in Australian hospitals has created two major sources of waste, confusion and fatigue for care teams: burgeoning patient data and alarm systems in the ward.
PATIENT DATA AND ALARM MANAGEMENT TRENDS FREE WEBINAR – 3PM, THURSDAY 27 AUGUST
REGISTRATION HERE
The emergence of digital systems in Australian hospitals has followed an eclectic and fraught path over the past two decades.
State by state, different major electronic health record (EHR) and patient administration system (PAS) vendors have fought hard for the major public hospital contracts. But depending on size, legacy systems, state funding and state-by-state strategy and organisation, the introduction of digital capability into Australian hospitals has been plagued by implementation issues, including integration with legacy systems.
Now, another issue is emerging as the base systems are surrounded by other bedside data generation from systems such as physiological monitors, ventilators, IV pumps, dialysis, nurse call and real-time care team location services.
One of the promises of a modern digital hospital setup is the simultaneous management of multiple patients with multiple data points, on many integrated and co-ordinated devices.
The reality has been a build-up of poorly integrated systems, working awkwardly with legacy systems, some of them still manual, and often in isolation from the core digital systems.
With multiple digital devices arriving at a patient’s bedside, each generating data for a particular aspect of their management and each usually having its own cascading alarm management protocol, the potential for fatigue and confusion among the care team is expanding rapidly.
The problem has spurned a whole emerging category of hospital consulting and integration services and products, in patient data and alarm management.
But such solutions aren’t that simple.
Care teams working in critical care environments are now being made less effective as a result of data overload.
EHR data provides a comprehensive view of the patient’s condition and status. But much of this data lacks situational relevance and is not provided to care teams in a timely enough manner or in the right context to be actionable.
Most often, real-time patient data is only available on the original medical devices that are connected to the patient at the point of care. And if many of these devices operate in this manner and are not integrated to a co-ordinated patient data flow protocol, the alarm fatigue and confusion can actually detract from the efficiency of existing teams.
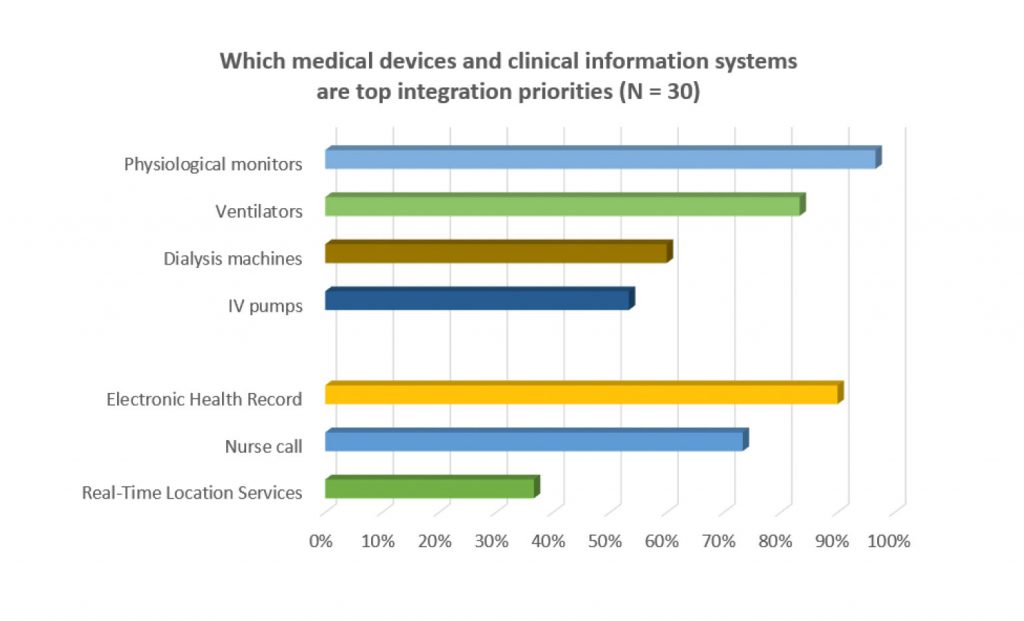
Yet in a recent Spyglass* survey of digitally enabled hospitals conducted in the past year, over 90% reported that there was enormous value to be had in better aggregating and presenting patient medical device data in clinical workflows that could inform better care decisions and better help co-ordinate care.
Hospitals in the survey reported that the highest priorities for such workflow improvement include reducing unnecessary interruptions to the care provider, improving response times via properly co-ordinated alarm protocols, more informed clinical decision making and an overall increase in provider efficiency.
A Wild Health webinar from 3pm to 4pm AEST on 27 August will talk to four experts in the field about what progress their hospitals and hospital networks have made in this important emerging area of digital development, the issues they currently face, and how they are planning to solve the increasing complexity their hospitals will face moving forward.
The expert panel includes:
- Patricia Liebke, Clinical Information Systems Lead, Ramsay Health
- Kate Renzenbrink, Chief Nursing and Information Officer, Bendigo Health
- Paolo Burchietti, Project Manager, Ascom UMS srl Information Technology & Services, Scandicci, Firenze, Italy
- Moderator: Jeremy Knibbs, Publisher, Wild Health and The Medical Republic
The panel will touch on:
- Volume of patient data
- Labour shortages and cost pressures
- Alert fatigue
- Physician and nurse burnout
- Care team communication in chronic care management
- Dealing with legacy
- Strategy of modelling for solutions in your context
- Prioritising in the context of identified issues
- The tools and products in play: predictive analytics, alarm
- Management, mobile, distributed dashboards,
- Unified communications
- Operationalising the ‘Silent ICU’, and
- ROI and investment planning
A third of the session with be devoted to audience Q&A.
REGISTER for FREE HERE and also receive the Spyglass Whitepaper on Trends in Patient Data and Alarm Management.
Administration queries on the webinar can be directed to talia@medicalrepublic.com.au.


