When certain treatments only have a small window of effectiveness and can reduce the benefits of other treatments, when is the best time to use them?
Long-term osteoporosis management requires you to consider fracture risk and individualised treatment options, according to an expert at last month’s World Congress on Menopause.
“We know that one of the best signs that your skeleton will fail in the future is that your skeleton has already failed,” Professor Eugene McCloskey, a rheumatologist from the University of Sheffield in the UK, told a plenary session.
“So, we want to take strategies that identify patients at increased risk of fracture and target them [with an] intervention that will decrease that future risk.”
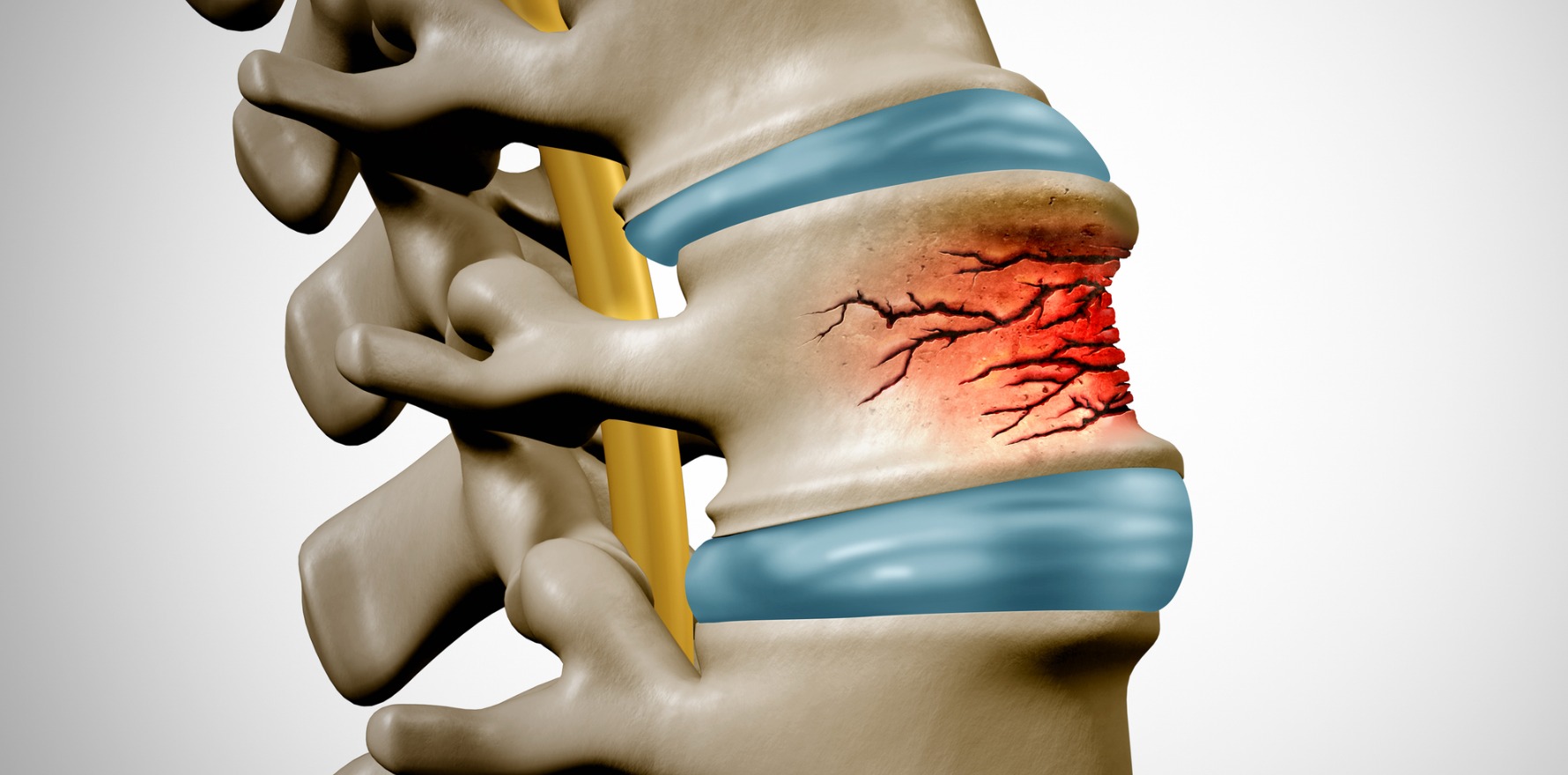
Fragility fractures associated with osteoporosis are the fourth-highest burden of years lived with disability, behind ischaemic heart disease, dementia and lung cancer, but the general medical community – and patients themselves – often fail to appreciate the true extent of the problem.
Managing fracture risk in osteoporosis comes down to two main things, according to Professor McCloskey.
The first is targeting lifestyle factors, which are similar advice to what is provided for other chronic diseases (i.e., managing body weight and obesity, increasing calcium and vitamin D intake, reducing alcohol intake and stopping smoking).
“[But] being Irish, it’s very difficult to define what moderate alcohol intake is,” Professor McCloskey added.
The second is the growing array of pharmacological treatments. These drugs typically fall into one of two classes: the antiresorptives (oestrogens, SERMs, bisphosphonates and RANKL targeted therapies) and the anabolics, or bone-forming agents (parathyroid peptides and antisclerostins).
“Although some of the more recent agents actually bridge both classes in that they have a dual action effect, and I’m specifically talking about romosozumab,” Professor McCloskey said.
But these drugs are not made to be equal, and the long-term pharmacological approach for minimising fracture risk is not as simple as putting a patient on one drug at age 50 and keeping them on it for the next 30 years.
Historically, he said, “we would go from the age of 50 through to 70 before we see anything other than antiresorptive treatments appearing in the treatment regimen.
“But we now know that high-risk patients, or very high-risk patients, aren’t all just 70 years and older. High risk and very high risk exist at earlier ages, [and] very low [bone mineral density] can exist at earlier ages. We might have to think about using bone-forming strategies up front in patients with those sorts of characteristics.”
Professor McCloskey highlighted two key studies that demonstrated the benefit of using a bone-forming agent before an antiresorptive: the VERO trial, which compared teriparatide and risedronate, and the ARCH trial, which compared romosozumab to alendronate. Both trials saw greater reductions in the incidence of new fractures when the bone-forming agent was used first.
“The initial treatment with the bone-forming treatment sets you off on a lower fracture trajectory than an antiresorptive agent, and that lower trajectory is maintained by following on treatment with an antiresorptive agent,” Professor McCloskey summarised.
“That’s allowed… anabolic treatments to be seen as first-line treatments in patients at very high risk [of fracture]. And that doesn’t just mean the elderly.”
However, using a combination of pharmacological approaches over an extended period of time creates its own set of challenges – such as how to safely and effectively transition from one medication to another.
Related
One challenging aspect of changing medications is that while most drugs only work for the time you take them, bisphosphonates continue to exert an effect for an extended period. This has benefits but isn’t without drawbacks. For example, the bone density-increasing effects of teriparatide and romosozumab are blunted if alendronate or other bisphosphonates are used before moving to a bone-forming agent. Prior treatment with denosumab has a similar effect.
“Even though romosozumab has an impact to reduce bone resorption, that’s still probably overwhelmed by the increase in bone resorption that ensures on stopping the denosumab,” Professor McCloskey told delegates.
A similar issue occurs for teriparatide.
“So, we need to think about denosumab [and] what might happen four or five or 10 years down the line – how am I going to manage if I need to stop or transition from denosumab to something else,” Professor McCloskey said.
Thankfully, the European Calcified Tissue Society has released a position statement on how to best manage taking a patient off denosumab. Professor McCloskey also recommended using zoledronate injections at six and 12 months after the last denosumab injection.