And countries that went hard with lockdowns and high rates of testing early on had far greater success controlling infection rates.
Welcome to The Medical Republic’s COVID Catch-Up.
It’s the day’s COVID-19 news in one convenient post. Email bianca@biancanogrady.com with any tips, comments or feedback.
6 November
- Asian ethnicity may be associated with greater risk of ischaemic stroke in COVID-19, study suggests.
- Control measures and testing decide national COVID-19 outcomes, not government capacity to respond.
- Latest COVID-19 testing numbers from around Australia show no cases of community transmission.
- Ischaemic stroke associated with COVID-19 may disproportionately affect people of Asian ethnicity, according to a study published in the Journal of Neurology, Neurosurgery and Psychiatry.
Researchers examined 1507 stroke admissions from March through to June, 86 of which occurred in patients who tested positive for SARS-CoV-2 at the time of stroke or shortly after.
They found that the number of Asian stroke patients was twice as high among the COVID-19 group compared to controls, which was entirely attributable to ischaemic strokes.
Patients with COVID-19 who experienced stroke also had significantly higher mean D-dimer levels compared to those without COVID-19, and ischaemic strokes were significantly more severe in patients with COVID-19 compared to those without. Significantly more ischaemic strokes resulted in death among those with COVID-19 than in controls.
“Our study provides the most compelling evidence yet that COVID-19-associated ischaemic strokes are more severe and more likely to result in severe disability or death, although the outlook is not quite as bleak as previous studies have suggested,” the authors wrote.
They suggested that all patients presenting with ischaemic stroke and very elevated D-dimer should be considered for SARS-CoV-2 testing, and that criteria for CT angiography should consider whether they have COVID-19. - Countries that went hard with lockdowns and high rates of testing early in the pandemic had far greater success controlling infection rates – regardless of their inherent health system capacity to respond – than did countries with more robust health systems that didn’t implement stringent control measures.
That’s the conclusion of an Australian study, published in the International Journal for Quality in Healthcare, which compared 40 health systems around the world on their capacity to respond, response stringency, scope of COVID-19 testing, and COVID-19 outcomes.
Government’s capacity to respond took into account aspects such as government policy stability, responsiveness to change, long term vision for the future, and economic strength and competitiveness.
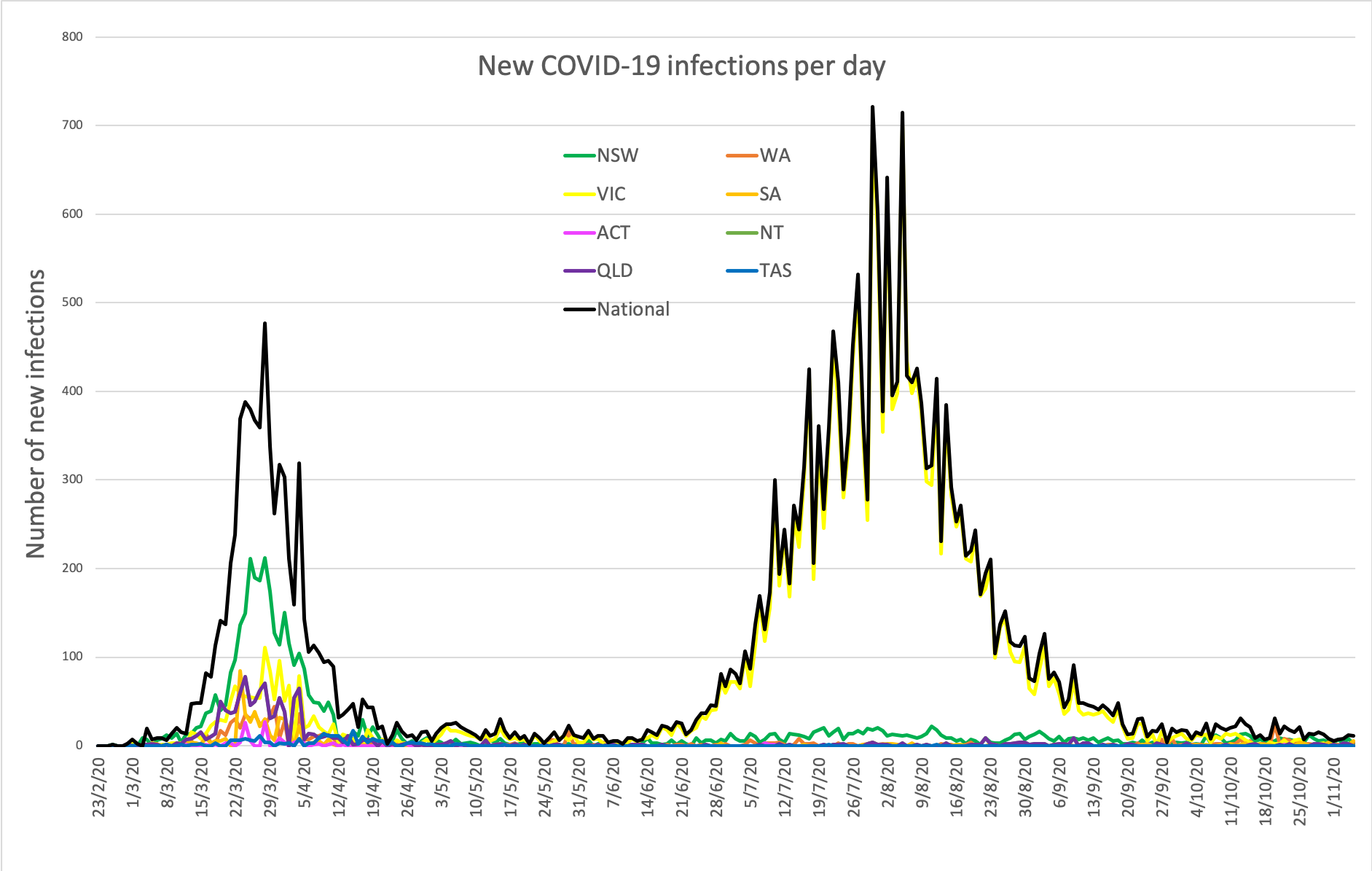
However the study found that this had little relation to the stringency of a government’s response to the pandemic or to death rates. The most important factors were how governments responded and how much testing was done. Governments that adopted more stringent lockdown measures and higher testing rates showing much lower death rates than those who adopted less stringent responses and tested less. - South Australia’s five new cases of COVID-19, Western Australia’s four new cases and New South Wales’ two new cases are all returned travellers in hotel quarantine. No new cases of community transmission were reported anywhere in Australia yesterday, and that is definitely cause for celebration.
Here are the latest confirmed COVID-19 infection numbers from around Australia to 9pm Thursday:
National – 27,633, with 907 deaths
ACT – 114 (0)
NSW – 4445 (2)
NT – 38 (0)
QLD – 1177 (0)
SA – 509 (5)
TAS – 230 (0)
VIC – 20,345 (0)
WA – 775 (4)