Nightclubs, music and food festivals, carnivals and schoolies festivals are some of the ‘very high-risk’ environments for spreading COVID-19 which should not be operating in the current stage of pandemic restrictions, government health body says.
Welcome to The Medical Republic‘s COVID Catch-Up.
It’s the day’s COVID-19 news into one convenient post. Email bianca@biancanogrady.com with any tips, comments or feedback.
3 September
- Festivals, nightclubs and carnivals are too high risk for this stage of COVID-19, says government health body.
- AMA releases guide to creating a COVID-safe medical practice.
- Is two weeks of isolation after a positive COVID-19 test enough? Possibly not, study suggests.
- WHO recommends systemic corticosteroid use for severe and critical COVID-19.
- Latest confirmed COVID-19 infection numbers from around Australia.
- Nightclubs, music and food festivals, carnivals and schoolies festivals are some of the ‘very high-risk’ environments for spreading COVID-19 which should not be operating in the current stage of pandemic restrictions, says the federal government’s health advisory committee.
The Australian Health Protection Principal Committee – which is made up of the state and territory chief health officers and chaired by the Chief Medical Officer – has singled out these and other activities such as community sporting events and unticketed spectator events as high-risk because of factors such as large numbers of people in close proximity, queueing, loud volume speech and singing, service of alcohol, and the risk of the virus being on surfaces that lots of people touch.
There’s a notable absence from the list: professional sporting events. Can’t imagine why. - The AMA has released a guide for how to have a COVID-safe medical practice, which covers issues such as maintaining physical distancing, cleaning and hygiene practices, PPE, and how to manage a staff member diagnosed with or a close contact of COVID-19.
- Two weeks of isolation after a positive COVID-19 test may not be long enough, say the authors of a study which has found the median time to viral clearance is 36 days after the onset of symptoms.
A paper published in BMJ Open presented the results of a retrospective cohort study involving 1162 individuals in Italy who tested positive for SARS-CoV-2 and were followed for at least 30 days after the initial test with further tests for the presence of viral RNA.
Overall 60.6% of patients were found to have cleared the virus, but a second swab only confirmed this for 78.7% of those patients, suggesting that around one in six negative result was false.
The median time to viral clearance was 30 days from the first positive swab, and 36 days from symptom onset. However this time increased with increasing age and disease severity.
The authors noted that detection of viral RNA didn’t necessarily mean the patient was infectious, but they also commented that evidence about the risk of transmission during the convalescent phase was weak, and serological data wasn’t adding much to the picture.
“Our data indicate that testing at 14 days from diagnosis, as many regional surveillance protocols recommend, will result in most cases still being positive,” the authors wrote, recommending that testing should be done more than four weeks after diagnosis to reduce the risk of false negatives.
They also commented that the WHO recommendations about the duration of isolation means that most individuals will still test positive for SARS-CoV-2 at the end of that two-week isolation period.
“Since there is still uncertainty regarding whether these same patients are infectious, our results have relevant public health implications.” - The case for corticosteroids in patients with severe and critical COVID-19 is building, with the World Health Organisation now recommending the use of systemic corticosteroids in these patients.
The recommendation was based on moderate certainty evidence, although in its recommendation the WHO noted that some members of the advisory panel expressed concern about the lack of clinical trial data on potential harms of corticosteroid treatment.
The WHO advised against using corticosteroids to treat non-severe COVID-19 based on the observation that there wasn’t strong evidence that corticosteroids in these patients achieved significant improvements in mortality.
A systematic review and meta-analysis, published in JAMA, has also found systemic corticosteroids are associated with lower 30-day mortality compared to usual care or placebo.
The meta-analysis of seven randomised controlled trials of systemic corticosteroids – dexamethasone, hydrocortisone, and methylprednisolone – found an overall 34% lower odds of all-cause mortality with any of these treatment options in critically ill patients.
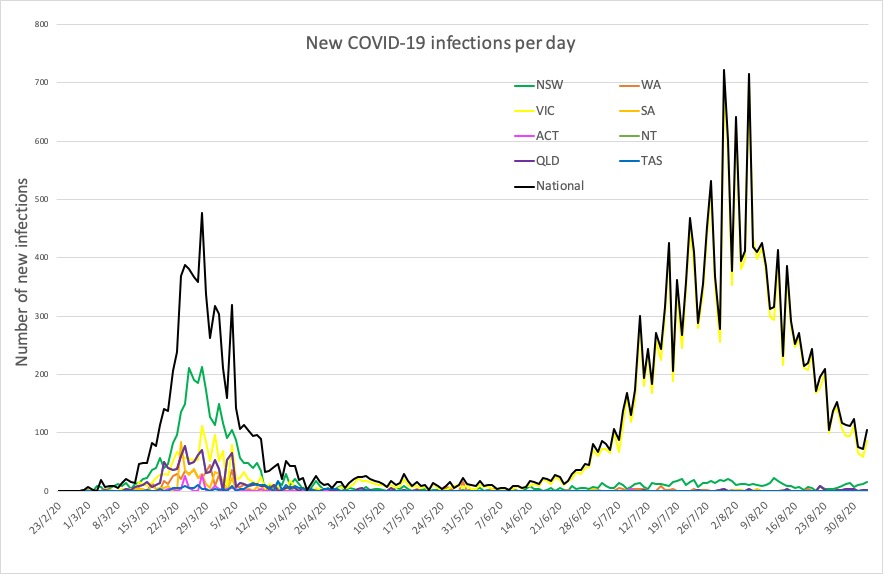
The most significant effects were seen with dexamethasone, which was associated with a 36% lower odds of all-cause mortality. Hydrocortisone was associated with a non-significant 31% reduction, and methylprednisolone was associated with a non-significant 9% lower odds. - Here are the latest confirmed COVID-19 infection numbers from around Australia to 9pm Wednesday:
National – 25,923, with 663 deaths
ACT – 113 (0)
NSW – 4079 (17)
NT – 33 (0)
QLD – 1126 (2)
SA – 463 (0)
TAS – 230 (0)
VIC – 19,224 (90)
WA – 655 (0)