And Pfizer boosters are now recommended for 16-17-year-olds.
Welcome to The Medical Republic’s Covid Catch-Up.
It’s the latest covid-19 news in one convenient post. Email bianca@biancanogrady.com with tips, comments or suggestions.
3 February
- Omicron’s secondary attack rate in households is 50%, study finds.
- Pfizer boosters now recommended for 16-17-year-olds.
- Childhood trauma could underpin rejection of covid public health measures.
- First human challenge trial with SARS-CoV-2 sheds light on viral dynamics.
- Global infection rates steady but deaths increasing.
- 574 deaths from covid in Australia in the past week.
Omicron’s secondary attack rate in households is around 50% and the average incubation period for the virus is 2.5-4.3 days, a study has found.
Writing in Emerging Infectious Disease, Korean researchers reported the results of a study involving 25 households with an index case and a total of 55 household members, and 12 household transmission pairs in November and December 2021.
They found that the overall secondary attack rate was 50%, which is higher than that seen for previous variants. The average serial interval – the time between the first case developing symptoms and the second case developing symptoms – was just 2.9 days, shorter than that seen for the wild type virus and Delta variant.
Pfizer boosters are now recommended for those aged 16-17 years, and can be given from three months after their second vaccine dose, ATAGI advises.
Those who were aged under 16 at the time of their second dose are also eligible for the booster. Anyone in that age group who is severely immunocompromised and has had three doses of vaccine can get the booster/fourth dose from three months after their third dose.
If adolescents have recently experienced covid infection, they should still get a booster within four months of recovering from acute infection.
Meanwhile, Pfizer has applied for emergency use authorisation for its vaccine in children aged six months to four years, which it did at the request of the US Food and Drug Administration. The agency will meet on 15 February to discuss the data.
Childhood trauma may contribute to rejection of public health measures designed to prevent covid, including mask-wearing, social distancing and vaccination, new research suggests.
A paper published in the BMJ reported the outcomes of a national cross-sectional study involving more than 2200 Welsh residents surveyed by telephone, who were asked about their attitudes to covid public health measures, trust in the National Health Service’s covid information, and adverse childhood experiences.
Researchers found those who had experienced adverse events in childhood – which included abuse, domestic violence, parent separation or living with a parent with drug or alcohol problems – were more likely to have low trust of the NHS, to feel unfairly restricted by governments, to want an end to mask requirements and to support the removal of social distancing.
Those who had experienced a lot of childhood trauma were four times more likely to be vaccine-hesitant than those with no experience of childhood trauma.
The authors also pointed out that people who had experienced childhood trauma were also at greater risk of poor health, poor mental wellbeing, and drug and alcohol use. “Without consideration of how best to engage such individuals, some risk being effectively excluded from population health interventions, remaining at higher risks of infection and posing a potential transmission risk to others,” they wrote.
Pour one out in honour of the thirty-four unvaccinated and infection-naïve individuals who volunteered to get infected with wild-type SARS-CoV-2, in the first human challenge trial for the virus.
Published in preprint form, the non-peer-reviewed study attempted to quantify just how much virus people needed to be exposed to to get infected, and what happened when they did.
Of the 36 who were exposed to the virus, in the form of intranasal drops, just over half developed PCR-confirmed infection. They began shedding virus from 40 hours after exposure, and viral loads peaked in the throat around five days later then in the nose at around six days later.
It took an average of 8.7 days to reach the point where viable virus was no longer detected in the throat, and 10.2 days until it was no longer detected in the nose.
Fortunately for those involved, none experienced severe disease and none required “rescue therapy”.
Global infection rates have remained steady for a second week, but deaths have increased by 9% over the previous week, according to the latest WHO update.
Covid case numbers are still accelerating upwards in Europe, the western Pacific – which includes Australia – and eastern Mediterranean region. Germany reported a 48% increase in cases compared to the previous week, and Brazil a 56% increase.
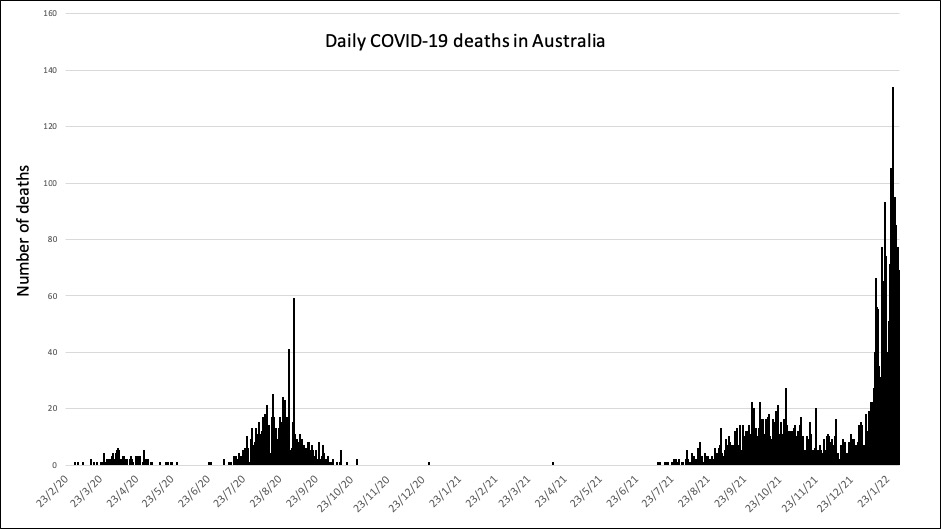
Five hundred and seventy four Australians died of covid in the past week, which is more deaths than occurred in the first seven months of the pandemic.