And Paxlovid reduces hospitalisation and death in the unvaccinated by 90% when given in first three days of symptoms.
Welcome to The Medical Republic’s Covid News.
Here’s this week’s covid news from around Australia and the world.
28 April
- Half of people hospitalised for covid not recovered at one year.
- Early Paxlovid reduces risk of hospitalisation or death in unvaccinated people by nearly 90%.
- Three-dose vaccine protection against Omicron drops significantly after three months.
- Omicron in pregnancy linked to lower risk of severe illness than infection with Delta or earlier variants.
- Global covid infections still dropping around the world, but rising again in the US and Africa.
Nearly half of people hospitalised for covid are still not recovered one year after discharge, and they are also more likely to have markers of persistent inflammation and damaged mucosal epithelium.
A longitudinal study, published in the Lancet Respiratory Medicine, of 807 people discharged from hospital after covid found that one year later nearly 49% said they were not recovered from the disease.
Women were 32% less likely to have fully recovered at one year than men; those with a BMI at or above 30 were 50% less likely to have fully recovered; and mechanical ventilation during hospitalisation was also associated with a greater risk of persistent symptoms at one year.
The most commonly reported symptoms were fatigue, aching muscles, physically slowing down, poor sleep, breathlessness, joint pain or swelling, slowing down in thinking, pain, short-term memory loss and limb weakness.
The study also looked at symptoms at five months after discharge and found nearly 20% of patients reported very severe mental or physical impairment and 30% reported severe mental or physical impairment.
When researchers analysed the proteome of 626 participants, they found 13 proteins that were significantly elevated among people with long covid, including those associated with inflammation – including neuroinflammation – and damaged mucosal epithelium.
The antiviral combination of nirmatrelvir plus ritonavir – sold as Paxlovid – is associated with a nearly 90% reduction in the risk of covid hospitalisation or death in unvaccinated individuals, if given within three days of symptom onset, new research shows.
A paper published in the New England Journal of Medicine reports the outcomes of a randomised placebo-controlled trial involving 1379 unvaccinated adults with symptomatic covid and at high risk of severe disease.
Researchers saw an 88.9% reduction in the risk of hospitalisation or death among patients treated with Paxlovid, with no deaths occurring in the treatment group. Among those treated within five days of the start of symptoms, there was a nearly 88% reduction in the risk of death or hospitalisation.
The most common adverse event seen among the treated group was change in taste, and the overall rate of adverse events was similar between the treatment and placebo arms of the study.
In Australia, the antiviral will be available on the PBS from 1 May (this Sunday) for people with mild to moderate confirmed covid and who have risk factors for severe disease. These include being over 65 years and with at least two risk factors for severe disease; over 75 and with at least one risk factor; being over 50 and of Aboriginal or Torres Strait Islander origin and with at least two risk factors; or being moderately to severely immunocompromised.
The drug must be given within five days of developing symptoms, and consists of two tablets taken together twice a day for five days.
Protection against hospitalisation from Omicron from three doses of the Pfizer vaccine drops significantly three months after the booster dose, according to a paper published in the Lancet Respiratory Medicine.
A study of 7361 people presenting to hospital with covid infection – nearly two-thirds of whom had Omicron, the rest Delta – found that the level of protection against hospital admission from Delta remained fairly high at least to six months after three doses of Pfizer vaccine.
However, the level of protection against hospitalisation from Omicron from three doses of vaccine waned from around 85% up to three months after the third dose to 55% after three months. Protection against emergency department admission with Omicron dropped from 77% less than three months after the third dose to 53% after three months.
Omicron infection during pregnancy carries a lower risk of severe illness than Delta or earlier variants, but similar risk of neonatal positivity, researchers have found.
A prospective study of 2641 SARS-CoV-2 infections diagnosed in pregnancy, published in JAMA, reported that while the incidence of covid during pregnancy was higher during the Delta and Omicron waves compared to with previous variants, Omicron was associated with an 80% lower odds of severe or critical illness, even after adjusting for vaccination.
In contrast, Delta infection during pregnancy was associated with a nearly three-fold greater odds of severe or critical illness compared to pre-Delta infections.
Of the 1919 infants delivered, just over 3% tested positive for SARS-CoV-2 and there were no significant differences in the risk of neonatal positivity between variants.
The rate of new covid infections continues to decline around the world, despite a 21% increase in new infections in the US and 32% increase in cases across Africa.
The latest WHO infection figures also show a continued decline in deaths from covid, which are now at the lowest level since March 2020 when the first wave of the pandemic struck.
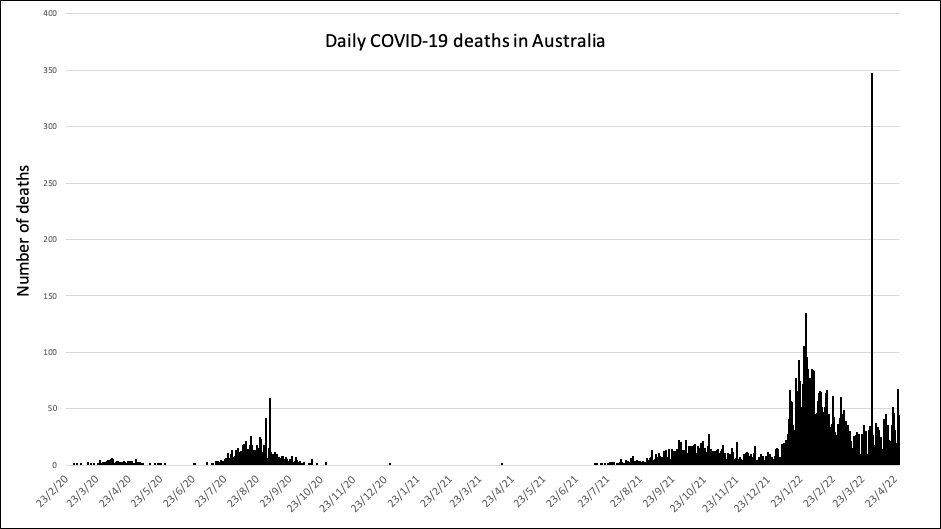
In Australia, covid has claimed 271 lives in the past week, bringing the total number of deaths in the pandemic so far to 7113.