And "fully vaccinated" status may be redefined to include boosters.
Welcome to The Medical Republic’s Covid Catch-Up.
It’s the latest covid-19 news in one convenient post. Email bianca@biancanogrady.com with tips, comments or suggestions.
27 January
- Age, asthma and severe covid are key risk factors for long covid.
- National Cabinet to consider redefining “fully vaccinated” amid calls for them to address inequities in public health measures.
- Three-quarters of those who survive ICU with covid have persistent physical symptoms one year later.
- Federal government wants NDIS participants to spend their own funds on RATs.
- Two monoclonal antibody treatments lose FDA authorisation over lack of effect against Omicron.
- Global data suggests latest covid surge could be slowing.
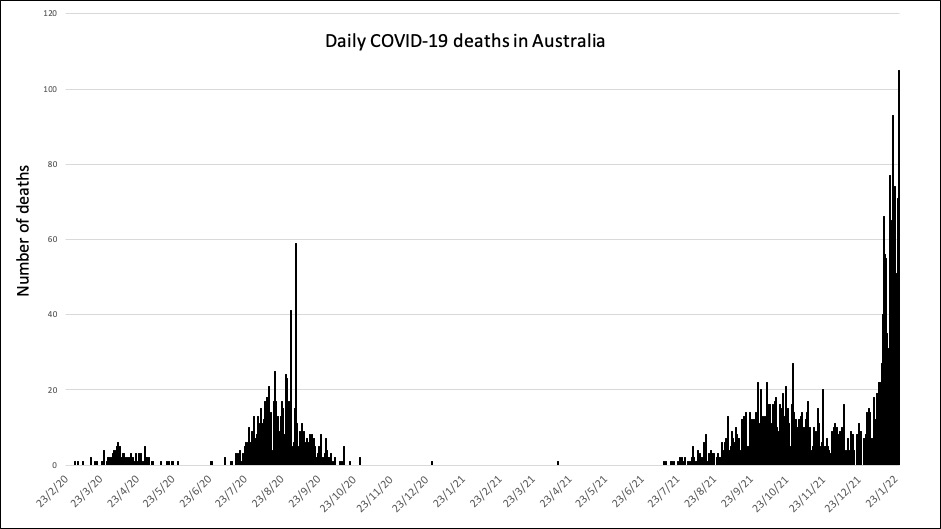
- Over one hundred Australian deaths from covid reported yesterday.
People with asthma appear to be at greater risk of long covid regardless of the severity of their initial covid infection, researchers have found.
A study published in Nature Communications followed 134 people with confirmed SARS-CoV-2 infection – ranging from asymptomatic cases to severe ARDS – for up to one year after their infection, and compared their symptoms and immunological profile to those of 40 healthy controls.
Overall, nearly 54% of those with mild covid and 82% of those with severe covid met the criteria for long covid. The study defined long covid as the persistence of one or more covid-related symptoms – most commonly fatigue, breathlessness, change in smell or taste, or anxiety or depression – for more than four weeks after the onset of symptoms.
Those who developed long covid were more likely to have experienced severe covid and have more covid symptoms during their acute infection, were older and more likely to have been hospitalised. Those with a history of lung disease had a six-fold higher odds of developing long covid, while those with a history of asthma had a nearly 10-fold higher risk.
Among individuals with a history of asthma, 94% still had covid symptoms at one month, and 71% had symptoms at one year after infection.
The National Cabinet meeting today is expected to address the question of whether the definition of “fully vaccinated” needs to encompass boosters, but some are urging greater consideration of the widening inequities during the pandemic, such as access to RATs, vaccines and support.
The Australian Council of Social Service issued a statement calling on the National Cabinet to address the disproportionate impact of the pandemic on people of low income, from marginalised and disadvantaged backgrounds, and with pre-existing vulnerabilities.
In particular, they highlighted the “huge gap” in booster uptake between high income and low income communities, and the fact that many people with concession cards still can’t access free rapid antigen tests despite the federal government committing to providing them.
“ACOSS calls for the creation of a civil society COVID Rapid Response Group consisting of ACOSS, unions, business peaks and public health experts to work closely with government to implement a range of policy measures and actions to protect those most at risk,” ACOSS CEO Dr Cassandra Goldie said in a statement.
Nearly three-quarters of patients treated in intensive care for covid are still experiencing physical symptoms including fatigue, weakness, joint and muscle pain and breathlessness one year after leaving the ICU.
Writing in JAMA, researchers report the findings of a prospective cohort study involving 246 patients who were still alive one year after admission to intensive care for covid.
At follow-up, 74% reported physical symptoms, 26% reported mental symptoms and 16% reported cognitive symptoms, with 30% still experience symptoms in at least two of these domains. More than half of those who had been employed before getting sick said they still had work-related problems, such as needing to work less hours or still being on sick leave.
The most common mental symptoms were anxiety and depression, but one in ten reported post-traumatic stress disorder symptoms.
However the prevalence of these persistent symptoms is on par with that seen in ICU survivors not admitted for covid, although the covid survivors had a higher rate of work problems than non-covid patients.
From the government that brought you the “Plunder Your Retirement Savings to Survive Covid” plan comes another stroke of fiscal bastardry: suggesting that some people on the National Disability Insurance Scheme use their NDIS core funding to pay for rapid antigen tests for themselves and their carers.
“This is another example of how we are supporting participants to use their funding flexibly during the COVID-19 pandemic, to ensure they continue to receive the disability-related supports they need,” Senator Linda Reynolds, minister for the NDIS, said in a statement.
Given that UK data from pre-Omicron suggested around 60% of deaths from covid were in people with disabilities, and given the criticism levelled at the federal government’s failure to successfully prioritise people with disabilities in the vaccine rollout, one might hope that easy and free access to rapid antigen tests for all NDIS participants might be the least the government could do to improve its track record.
Rapid antigen tests are funded for NDIS participants in supported independent living – at least until next week – and for concession card holders, but that still leaves around 18% of NDIS participants with no subsidised or funded access to RATs.
The Guardian reported that some NDIS participants were spending up to $1000 for rapid antigen tests for their carers, and questioned whether NDIS core funding would be increased to cover the cost of purchasing RATs.
The US Food and Drug Administration has withdrawn its authorisation for two monoclonal antibody covid treatments – bamlanivimab plus etesevimab and REGEN-COV (casirivimab and imdevimab) – because of research suggesting they don’t work against Omicron.
However they have left the door open to re-authorising the therapies if a new variant emerges that is susceptible to their mode of action.
A 5% increase in new covid infections globally in the past week could signal an approaching peak of the Omicron surge, even as weekly records continue to be set.
The latest WHO update reports 21 million new cases were diagnosed in the past week, although deaths have plateaued at around 50,000.
The European region continues to account for the greatest percentage of new infections, with France recording a 21% increase in infections and Italy a 24% increase.
Australia recorded more than 100 deaths from covid yesterday, marking a grim new record for the pandemic. One hundred and five deaths were reported, including 29 in New South Wales, 35 in Victoria, nine in Queensland and 13 in South Australia.