The finding has implications for seroprevalance studies, which may underestimate the true number of people infected with SARS-CoV-2.
Welcome to The Medical Republic’s COVID Catch-Up.
It’s the day’s COVID-19 news in one convenient post. Email bianca@biancanogrady.com with any tips, comments or feedback.
26 November
- One in four with mild COVID-19 may lose antibodies within months.
- More than half of intubated COVID-19 patients survive to hospital discharge, study finds.
- Comparison of mask-wearing and non-mask-wearing counties shows significant impact on infection rates.
- Many of world’s most connected cities at high risk of zoonotic pathogen spillover.
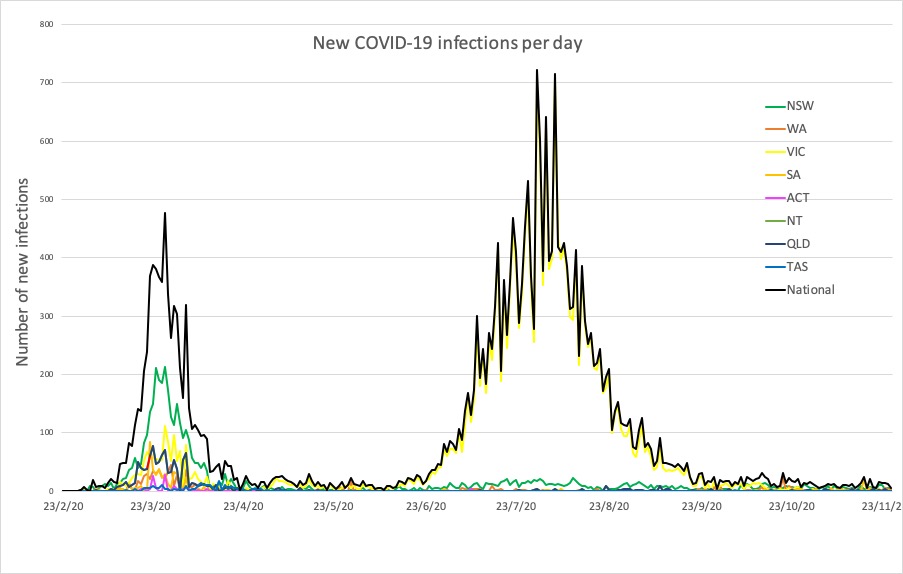
- Latest confirmed COVID-19 infection rates from around Australia.
- Around one in four individuals with mild COVID-19 infection may have no detectable antibodies to the virus within a couple of months, research suggests.
A study published in Morbidity and Mortality Weekly Report examined antibody levels in 3,248 healthcare workers, 156 of whom tested positive for SARS-CoV-2 antibodies at baseline. Two-thirds of these had experienced symptoms of COVID-19 infection, but none had been hospitalised.
At 60 days after baseline testing, antibodies levels had declined in nearly 94% of participants, and in 28% the levels dropped so low they fell below the threshold for positivity.
Participants who had experienced COVID-19 signs or symptoms were less likely to serorevert below positive antibody levels than those who didn’t experience symptoms. Similarly, those with higher initial antibody responses at baseline were less likely to serorevert than those with low initial antibody levels.
“These results suggest that a substantial proportion of persons infected with SARS-CoV-2 might have negative serologic test results in the months following infection,” the authors wrote.
They commented that this finding has implications for seroprevalance studies, as these may underestimate the true number of people infected with SARS-CoV-2. - More than half of intubated COVID-19 patients survive to be discharged from hospital, according to a cohort study published in PLOS ONE.
Researchers analysed data from five hospitals in Virginia, US, where a total of 1023 COVID-19 positive patients were admitted to hospital and 164 of these were placed on invasive mechanical ventilation.
Overall, 57% of the mechanically-ventilated patients survived to discharge. There was a significant age difference between those who survived and those who did not – with a median age of 55 years and 67 years respectively – and those who died also had significantly higher initial d-dimer levels and peak ferritin levels.
Around one-quarter of patients were intubated on the day of admission, and on average patients were ventilated for 14.6 days.
“We feel it is particularly reassuring that the death rate in our cohort was not higher, given our system strategy of avoiding intubation unless patients were truly unable to maintain their oxygenation or ventilation despite aggressive management with non-invasive measures,” the authors wrote. “Given this approach, the cohort of patients managed with IMV was likely sicker than those reported in some of series and could be expected to have less favorable outcomes.” - Kansas counties that made mask-wearing compulsory experienced a decline in the incidence of COVID-19 after introducing the mandate, while those that didn’t experienced an increase in COVID-19 incidence, a study has found.
Writing in Morbidity and Mortality Weekly Report, researchers reported on the impact of mask-wearing practices across the 105 counties of Kansas in the US.
The Kansas governor issued an executive order on July 3 requiring mask wearing in all public spaces, however only 24 counties complied with the order, providing a unique opportunity to compare the effect.
Among counties that adopted the mask mandate, the incidence of COVID-19 decreased by 6% from July 3 to August 23, while those that did not require masks in public places had a 100% increase in incadence.
The only other mitigation strategy that was adopted across Kansas during this time related to schools, but even after adjusting for other county-level differences in public health initiatives, the effect of mask-wearing on incidence remained. - Here’s a cheery thought: around 40% of the world’s most connected cities are found in areas where there is a high risk of zoonotic pathogens ‘spilling over’ from animals to humans.
A study published in OneHealth looked at the animal-health interface zones within 50 kilometres of the most highly connected cities around the world – cities whose airports are most central to global air traffic.
They found that 40% of the most connected quartile of cities were within 50 kms of zones with the highest risk of human-animal interaction that could result in pathogens being spread. Many of these cities were also in countries with poor health system performance and therefore less able to detect emerging pathogens and prevent their spread. - While the four new cases in New South Wales reported yesterday were all returned travellers in hotel quarantine, NSW Health has issued a COVID-19 alert for south-west Sydney following the detection of SARS-CoV-2 RNA fragments in wastewater at Liverpool.
Here are the latest confirmed COVID-19 infection numbers from around Australia to 9pm Wednesday:
National – 27,854 with 907 deaths
ACT – 115 (0)
NSW – 4552 (4)
NT – 47 (0)
QLD – 1197 (0)
SA – 558 (0)
TAS – 230 (0)
VIC – 20,345 (0)
WA – 810 (2)