The National COVID-19 Clinical Evidence Taskforce has released updated guidelines for GPs on the management of patients with suspected mild COVID-19
Thanks for joining us today on The Medical Republic‘s live COVID-19 blog.
Thank you to our sponsor and supporter for funding this project with an independent grant, Boehringer Ingelheim.
The latest
- Updated Australian guidelines on management of mild COVID-19
- Royal Flying Doctors get $38 million funding boost for COVID-19 response.
- Australia’s actions on COVID-19 have avoided public health crisis, say researchers.
- The National COVID-19 Clinical Evidence Taskforce has released updated guidelines for GPs on the management of patients with suspected mild COVID-19.
The guidelines include detailed advice on baseline assessment, supportive care, therapies for pre-existing conditions, escalation of care and release from isolation.
The advice on baseline assessment is that no investigations are required for mild disease, and chest x-ray or blood tests should only be performed if clinically indicated. Patients with mild disease can be managed in the community if given advice on symptom management and self-isolation, and are checked on by someone else if they are living alone.
The advice for managing mild COVID-19 in people with asthma or COPD is that they should continue their existing dosage of preventer medication or inhaled corticosteroids, but metered dose inhalers is preferred over nebulisers.
Similarly, the guidelines recommend patients with diabetes or cardiovascular disease continue on their current medication dosages, while patients on immunosuppressive therapies should also continue their treatment as before.
The authors advise that if symptoms do worsen, this is most likely to occur in the second or third week of illness, and patients should go to hospital if they show symptoms such as severe shortness of breath, blue lips or face, chest pain or pressure, coughing up blood, or signs of pneumonia.
3.25pm, 20 April
Please enjoy some excellent data visualisation courtesy of TMR‘s Felicity Nelson:
People who have died of COVID-19 in NSW have mostly been in their 80s (32%) and 90s (39%), although 21% of deaths occurred in people in their 70s.
[covid-19-graph]DeathsbyageinNSWfromCOVID-19/Sheet5[/covid-19-graph]
While the rate of COVID-19 infections appears to be falling in the community, the rate of COVID-19-related hospitalisations, ICU admissions and tells a different story. Here’s the latest data from NSW Health showing that the number of people receiving care for COVID-19 remains relatively stable, meaning we’re not in the clear yet:
[covid-19-graph]COVID-19casesbeingtreatedinICUonventilatorsandimmediatedeaths/pressreleasedata[/covid-19-graph]
1.25pm, 20 April
- More than three million Australians have made use of telehealth items introduced by the federal government during the COVID-19 pandemic, according to an announcement from health minister Greg Hunt.
Since 13 March, 274 new MBS items have been created, including 28 new telehealth items for specialists and allied health professions that will be added today.
More than 4.3 million telehealth services have been delivered; more than 700,000 in the past week alone.
“Every patient who uses a telehealth service is helping to maintain social distancing and flatten the coronavirus curve in Australia,” Mr Hunt said in a statement.
He also said the health profession had worked in “genuine partnership” with the government to quickly develop and implement the new telehealth items.
“This is an extraordinary feat and a reflection of our doctors’ and allied health professionals’ commitment to delivering accessible, best-practice care for all patients, during this difficult time,” he said.
- The Royal Flying Doctor Service has been given a $38 million funding boost from the federal government boost to help rural and remote communities through the COVID-19 pandemic.
The money will go towards evacuating suspected or confirmed COVID-19 cases, expand existing telehealth services, deliver fly-in GP respiratory and testing clinics, and ensure there is enough personal protective equipment for frontline staff.
- The Doherty Institute has released an analysis of the Australian COVID-19 epidemic so far, suggesting that government and community action was taken early enough and with enough commitment to avoid a public health crisis.
The unpublished article examined the 6533 confirmed cases of COVID-19 as of 18 April, and estimated the effective reproduction number of the virus – how many new cases come from each infected patient – had likely dropped below 1 in each state since mid-March.
“Our analysis suggests that Australia’s combined strategy of early, targeted management of the risk of importation, case targeted interventions, and broad-scale social distancing measures applied prior to the onset of detected widespread community transmission has substantially mitigated the first wave of COVID-19,” the authors wrote.
They suggested that the Australian healthcare system was in good shape to handle projected COVID-19 case loads over the next two weeks, but that would still require ongoing assessment and monitoring of hospital and ICU demand, as well as vigilance for localised outbreaks.
The number of asymptomatic, mild and undiagnosed infections was still a largely unknown factor, the authors said, pointing out that if this number was high, relaxing lockdown measures could see a rapid rise in disease activity.
“There are difficult decisions ahead for governments, and for now Australia is one of the few countries fortunate enough to be able to plan the next steps from a position of relative calm as opposed to crisis,” they wrote.
- A study of healthcare workers infected with COVID-19 in the United States has found nearly two-thirds continued working despite experiencing symptoms.
A researcher letter published in JAMA reported symptom data from 48 healthcare workers based at 22 facilities – long-term care, outpatient clinics, and acute care hospitals – across King County, Washington, who tested positive for SARS-CoV-2.
Half of those surveyed reported cough, nearly 42% reported fever and just over one-third reported muscle aches. However eight individuals had no fever, cough, shortness of breath or sore throat, but did experience chills, ‘malaise’, muscle aches or stuffy nose.
The study reported that 31 of the participants worked between one and 10 days in their jobs while they were experiencing symptoms.
“The data indicate that HCP worked for several days while symptomatic, when, according to a growing body of evidence, they may transmit SARS-CoV-2 to vulnerable patients and other HCP,” the authors wrote.
They suggested expanding symptoms-based screening criteria and making testing easier for symptomatic healthcare workers, as well as “creating sick leave policies that are nonpunitive, flexible, and consistent with public health guidance.”
- The AMA has proposed a staged resumption of elective surgery, starting with low-risk high-benefit procedures as the Federal Government flags lifting the ban on elective surgery as early as this week.
Elective surgery was all but suspended in late March to free up resources to respond to the COVID-19 pandemic, with the only exemptions being patients who were otherwise likely to deteriorate to the point of needing emergency care.
However the ABC reports Federal Health minister Greg Hunt said over the weekend that the government would likely allow elective surgery and IVF to resume, depending on the outcome of a meeting with the Prime minister, premiers and chief ministers this week.
The AMA says that the success of Australia’s COVID-19 response so far means there is available capacity in both public and private hospital, and this suggests that elective surgery could be “cautiously and gradually” restarted.
“A gradual loosening of restrictions is also consistent with the Government’s and the AMA’s view that patients should not ignore existing health concerns, and seek medical care when needed,” said AMA President Dr Tony Bartone in a statement.
They have called for a graduated restart of all Category 2 elective surgeries – semi-urgent procedures for conditions that cause pain, dysfunction or disability but which are not likely to deteriorate quickly or become an emergency – including IVF procedures.
“Doctors should be authorised to make decisions about what surgeries can proceed in the best interests of patients and clinicians,” Dr Bartone said.
However he stressed that hospitals must have an adequate supply of personal protective equipment before undertaking any surgeries. - Did you miss anything significant over the weekend? Apart from the blazing cesspit that is the United States’ COVID-19 situation, it was fairly quiet, at least in Australia. No news is good news.
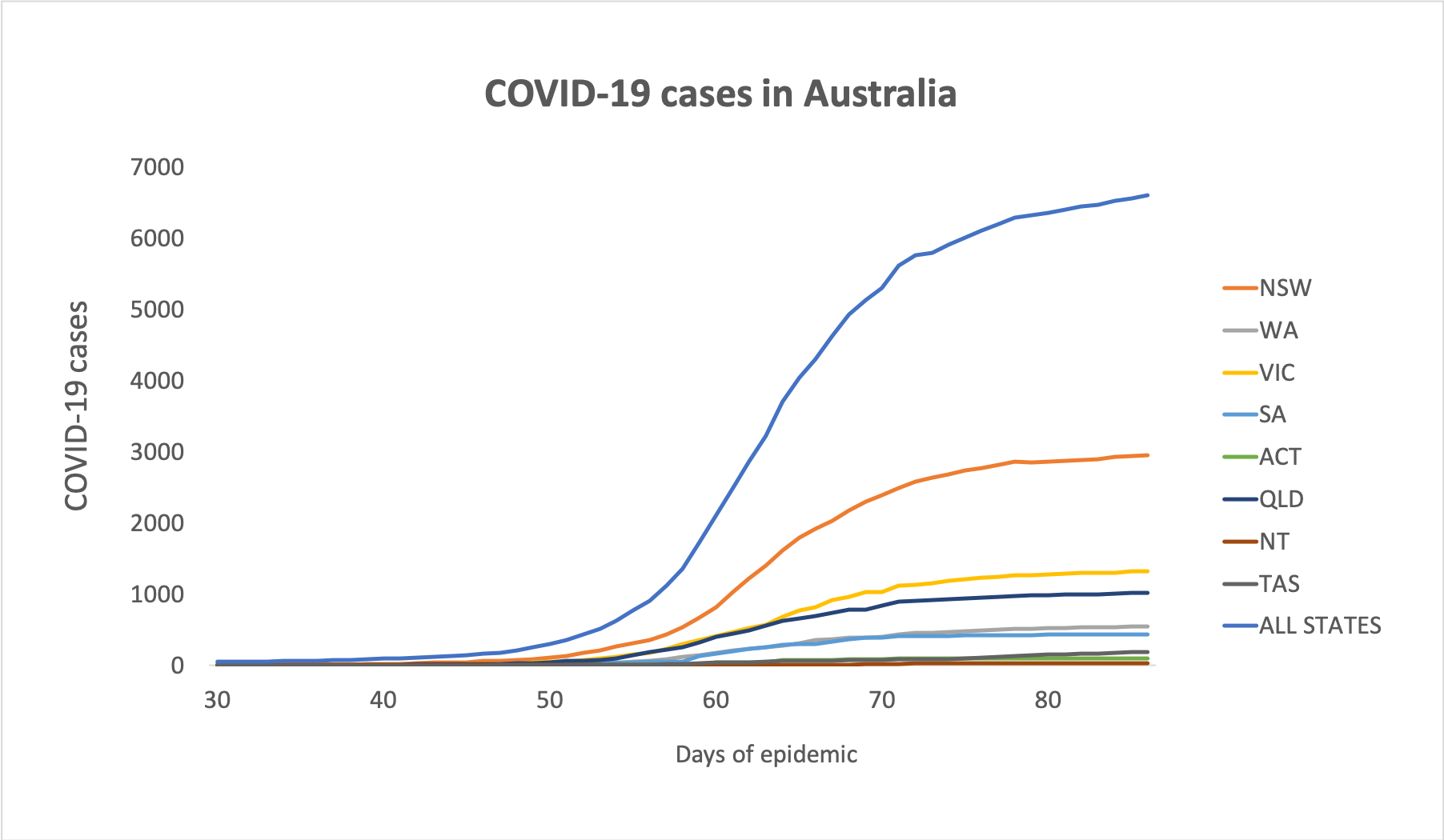
Here are the latest infection figures for Australia, to 3pm yesterday:
National – 6606 (up 41) and 70 deaths
ACT – 103
NSW – 2957
NT – 27
QLD – 1019
SA – 435
TAS – 192
VIC – 1328
Disclaimer: The content on the Medical Republic COVID-19 blog is independently created by Medical Republic without input from Boehringer Ingelheim Pty Ltd. The views, information, or opinions expressed on the Medical Republic COVID-19 blog are Medical Republic’s own and do not necessarily represent those of Boehringer Ingelheim Pty Ltd. Boehringer Ingelheim Pty Ltd is not responsible for and does not verify the accuracy of any content on the Medical Republic COVID-19 blog.


