Surgery in patients with COVID-19 is associated with a high risk of postoperative pulmonary complications, particularly in men and those aged over 70 years, new research suggests.
Thanks for joining us on The Medical Republic‘s live COVID-19 blog.
And thank you to our sponsor and supporter for funding this project with an independent grant, Boehringer Ingelheim.
The latest
- Afternoon update: High surgical complication rate in COVID-19 patients, brain imaging suggests viral invasion of olfactory regions in COVID-19.
- Morning update: COVID-19 motivating more to quit smoking, and TGA advice on sourcing PPE.
- Today’s updated COVID-19 infection figures for Australia
- Surgery in patients with COVID-19 is associated with a high risk of postoperative pulmonary complications, particularly in men and those aged over 70 years, new research suggests.
A paper published in The Lancet reported the findings of an international cohort study of 1128 surgical patients with confirmed SARS-CoV-2 infection, one quarter of whom were undergoing emergency surgery and the rest elective.
Around half the patients experienced pulmonary complications such as pneumonia, ARDS, or unexpected postoperative ventilation, and 38% of these patients died within 30 days of surgery. Thirty-day mortality risk was 75% higher in men, and 2.3-fold higher in those aged over 70 compared to those aged under 70.
“The increased risks associated with SARS-CoV-2 infection should be balanced against the risks of delaying surgery in individual patients,” the authors wrote. - At the height of the COVID-19 pandemic in Paris, the number of out of hospital cardiac arrests doubled, and around one-third of this increase was attributed to COVID-19 infections.
“Although this result might be partly related to COVID-19 infections, indirect effects associated with lockdown and adjustment of health-care services to the pandemic are probable,” researchers wrote in The Lancet: Public Health.
The population-based observational study used data from an ongoing database of non-traumatic out-of-hospital cardiac arrest in Paris and its suburbs to show the maximum weekly incidence of out-of-hospital cardiac arrest increased from around 13 before the pandemic started in mid-March to more than 26 during the pandemic’s peak, then returned to normal. - Magnetic resonance imaging of the brain of a woman with severe COVID-19-associated loss of smell and taste has found evidence of abnormalities suggesting viral invasion of the brain. A paper, published in JAMA Neurology, described changes to the regions of the brain associated with smell – the posterior gyrus rectus, for those with neurological interests – but which resolved over the course of the infection.
“Based on the MRI findings, including the slight olfactory bulb changes, we can speculate that SARS-CoV-2 might invade the brain through the olfactory pathway and cause an olfactory dysfunction of sensorineural origin; cerebrospinal fluid and pathology studies are required to confirm this hypothesis,” the authors wrote.
- The threat of COVID-19 appears to have motivated many smokers to quit, with a four-fold increase in the number of Australians downloading the government’s My Quitbuddy app, according to Federal Health Minister Greg Hunt.
The minister said that from January to May this year, the app was downloaded around 24,000 times, which was a ‘staggering’ increase over the same time last year.
“These figures are very encouraging and I congratulate those who have taken the first step,” Minister Hunt said in a statement.
He noted that while there was growing evidence that smokers were at greater risk of development severe COVID-19, the jury was still out on whether it also meant an increased risk of contracting the disease in the first place.
Meanwhile, the Australian Health Protection Principal Committee put out a statement late last week about smoking, e-cigarettes and COVID-19, which reiterated the importance of quitting smoking at any time, but particularly with the threat of COVID-19. On the question of e-cigarettes and COVID-19, AHPPC said that while there is currently no direct evidence on interactions between e-cigarette use and COVID-19 susceptibility or severity, there was increasing evidence that e-cigarettes use “poses a range of harms to the heart and lungs.” - The Therapeutic Goods Administration has reminded health professionals to only buy personal protective equipment that is listed on the Australian Register of Therapeutic Goods. They also warned that shortages of masks, gloves and gowns may occur, and that healthcare professionals should plan accordingly “in a composed manner” (so, no toilet-paper-panic-inspired punch-ups in the aisles please).
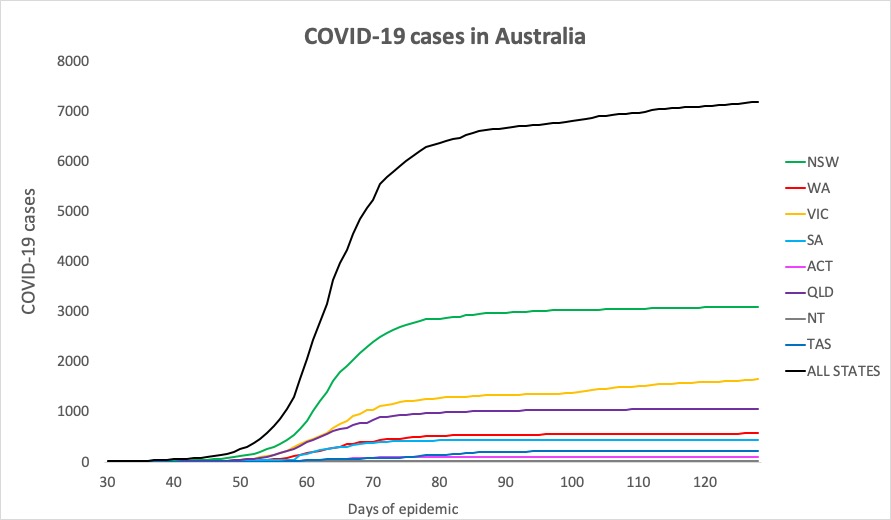
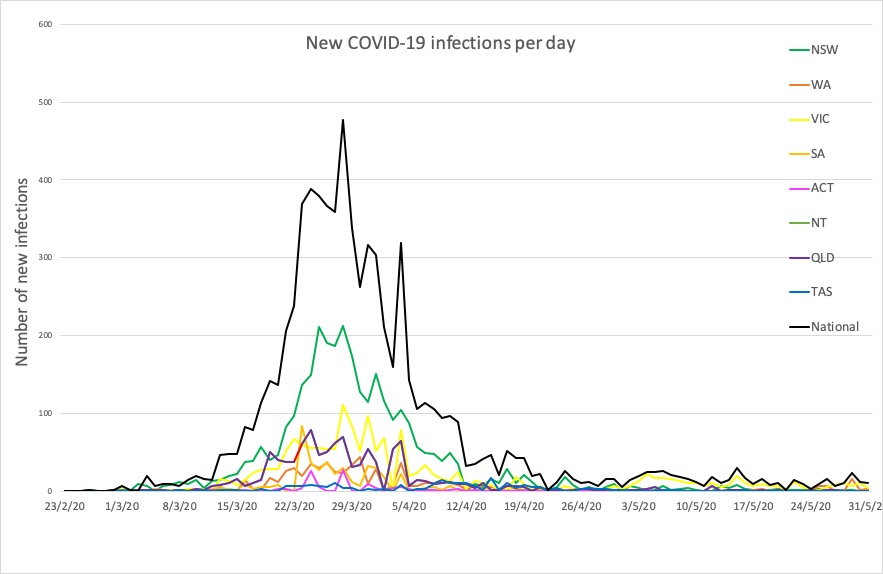
- Victoria and Western Australia are still showing the biggest increases in new infections. Western Australia’s new infections largely consist of returned travellers and the crew of an international vessel, while in Victoria, new cases have been linked to a family outbreak that now numbers 13 infections in total, and another case connected to the Rydges hotel in Swanston.
Here are today’s confirmed COVID-19 infection figures around Australia, to 9pm yesterday:
National – 7195, with 103 deaths and 6614 recovered
ACT – 107
NSW – 3095
NT – 29
QLD – 1058
SA – 440
TAS – 228
VIC – 1649
WA – 589
Disclaimer: The content on the Medical Republic COVID-19 blog is independently created by Medical Republic without input from Boehringer Ingelheim Pty Ltd. The views, information, or opinions expressed on the Medical Republic COVID-19 blog are Medical Republic’s own and do not necessarily represent those of Boehringer Ingelheim Pty Ltd. Boehringer Ingelheim Pty Ltd is not responsible for and does not verify the accuracy of any content on the Medical Republic COVID-19 blog.