The National Cabinet has met today and decided on a plan to get the country out of lockdown without unleashing a disastrous COVID-19 epidemic.
That’s it for today on The Medical Republic‘s live COVID-19 blog.
Thanks for joining us, and thanks to our sponsor and supporter for funding this project with an independent grant, Boehringer Ingelheim.
The latest
- Australians are worried that we’re drinking more than usual.
- Rapid point-of-care COVID-19 testing to be rolled out across rural and remote Aboriginal and Torres Strait Islander communities.
- Three goals need to be met before lifting COVID-19 restrictions, says PM.
- Times are tough, and Australians are hitting the bottle a little too much in trying to cope, says the Foundation for Alcohol Research and Education.
National polling commissioned by the organisation shows 70% of Australians are drinking more than usual, one in five Australians are buying more alcohol than usual during the pandemic, and one-third of those are worried about their drinking or someone else’s in their household.
“Increased drinking by people worried about COVID-19 might be good news for alcohol industry executives, but it’s certainly worrying news for our community’s health,” said FARE CEO Caterina Giorgi in a statement.
- A rapid point-of-care testing program is being funded for remote and rural Aboriginal and Torres Strait Islander communities.
Minister for Indigenous Australians Ken Wyatt announced a $3.3 million investment in 83 rapid COVID-19 testing sites across at-risk and in-need Indigenous communities, to be set up by mid-May.
“It has been developed in close consultation with Aboriginal Community Controlled Health Services and states and territories, which are actively involved in site selection and assessment to ensure no community is more than two to three hours’ drive from a testing facility,” Wyatt said in a statement.
The program – an initiative of the Kirby Institute in partnership with the Flinders University – will use the Xpert SARS-CoV-2 RT-PCR test to deliver point-of-care results in around 45 minutes. Currently in places like the Kimberley, test results can take up to 10 days.
- From TMR’s Penny Durham: The National Cabinet has met today and decided on a plan to get the country out of lockdown without unleashing a disastrous COVID-19 epidemic.
Prime Minister Scott Morrison said three goals needed to be met before restrictions could be lifted: an expanded sentinel testing regime; greater tracing capability; and local response capabilities such that sudden outbreaks like the current one in Burnie, northwest Tasmania, can be immediately contained.
He said there would be no lifting of restrictions over the next four weeks while these three elements were put in place.
Chief Medical Officer Brendan Murphy said the potential still existed for large and uncontrolled outbreaks.
“If we relax the distancing measures that are stopping or reducing community transmission, that will inevitably lead to more outbreaks,” he said.
“We cannot afford to relax until we have a public health system that is so finely tuned it can detect and respond to any outbreak. We’re not confident just yet that … we can guarantee to government that we can deal with any outbreak.
“We just have to hold the course until we get ourselves completely ready.”
Based on new “nowcasting” modelling from the Doherty Institute, Professor Murphy said the effective reproduction number in most states was now well below 1, meaning the epidemic was under control.
He said Australia had one of the highest symptomatic case detection rates in the world.
Professor Murphy and Mr Morrison reiterated the health advice was that children were safe at schools, since they were not great spreaders, but schools needed to implement distancing and hygiene to ensure the safety of teachers.
2.30pm, 16 April
- It looks like the many calls for Australians to get vaccinated against influenza are being heeded:
We have 13 million units of flu vaccine that have been released by the medical regulator.
2 million have been taken up so far.
That’s better than previous years at this time. https://t.co/XXc5LdXrot
— Greg Hunt (@GregHuntMP) April 16, 2020
- Got an idea for COVID-19-related research in general practice? The RACGP, in partnership with the HCF Research Foundation, is offering grants of up to $50,000 to support research projects relating to COVID-19 and general practice.
RACGP President Dr Harry Nespolon said in a statement that the research could examine subjects such as the use of telehealth and telehealth item numbers, how COVID-19 clinics are working, and the impact of COVID-19 on general practice.
Preference is given to research that collects data during the pandemic phase, but can also go to current research projects that can be adapted to cover COVID-19.
Applications for the grants close on Friday 24th April 2020, and details are here.
- Obese individuals in intensive care have a seven-fold higher odds of requiring invasive mechanical ventilation for COVID-19 than those in the healthy weight range, a study has found.
Writing in the journal Obesity, researchers report on the outcomes from 124 consecutive patients admitted to intensive care with COVID-19 in a single hospital in France, nearly 70% of whom required invasive mechanical ventilation.
The analysis showed that the need for ventilation increased significantly with increasing BMI, even after accounting for age, diabetes and hypertension. Around 85% of patients with severe obesity needed ventilation, compared to just under half of those with a BMI at or below 25 kg/m2.
The odds ratio for mechanical ventilation in severely obese patients was more than seven-fold higher than in healthy-weight patients, the study found.
- People with COVID-19 may be at their most infectious at or before symptoms begin and nearly half of human-to-human transmission may be occurring before symptom onset, a new study published in Nature Medicine suggests.
Researchers collected 414 throat swabs from 94 patients with laboratory-confirmed COVID-19, from symptom onset to 32 days after that. They found high viral loads were present shortly after symptoms began, which then decreased over the next few weeks.
At the same time, they looked at data from 77 transmission pairs – cases of confirmed transmission from one person to another with no reported exposure outside that contact. Assuming a mean incubation period of 5.2 days, which has been established in a previous study, this transmission pair data suggested that infectiousness began as early as 2.3 days before symptoms emerged, and reached a peak just after symptom onset.
Altogether, they estimated that 44% of human-to-human transmission was occurring in the presymptomatic period.
“More inclusive criteria for contact tracing to capture potential transmission events 2 to 3 days before symptom onset should be urgently considered for effective control of the outbreak,” the authors wrote.
- Australian researchers are recruiting people with compromised immunity and who have tested positive for COVID-19 for a study on how the infection interacts with an altered immune state.
The study, which is a collaboration between some of Australia’s biggest medical research organisations, is looking for people undergoing cancer treatment, who have received a solid organ or stem cell transplant, are living with HIV, have an inherited immunodeficiency or are taking immunomodulatory therapy, and who have tested positive for COVID-19.
Given that some of the complications of COVID-19 appear to relate to immune over-reaction that impacts the lungs, immunologist Dr Sarah Sasson from the Kirby Institute and Westmead Hospital said it was possible that immune therapies could reduce this overactive response.
“If through this study we identify a treatment that appears to be protective against severe COVID-19, we can rapidly move it into the controlled trials, the gold standard to test whether a new treatment works,” she said in a statement.
There are 30 clinical sites around Australia participating in the study, which is being coordinated by the Kirby Institute at UNSW Sydney.
- It’s a shit job but … Australian researchers have shown that SARS-CoV-2 can be detected in raw sewage, which could enable an early warning surveillance system and tracking community infections through wastewater monitoring.
Scientists from the University of Queensland and CSIRO examined wastewater samples from two treatment plants in south east Queensland, which process sewage from the Brisbane area, and were able to find fragments of SARS-CoV-2 RNA.
It’s only a proof-of-concept study, and there are still many questions to be answered – such as how the levels of RNA correlate with infection rates. However CSIRO Land and Water Science Director Dr Paul Bertsch said in a briefing that he believed this would be very important for the recovery phase of the pandemic, particularly for monitoring the effectiveness of different interventions.
- There was some interesting COVID-19 stuff on the preprint servers yesterday. A study found that children infected with COVID-19 show much lower rates of fever, cough, pneumonia and lymphopaenia than do adults. A retrospective study of patients with COVID-19 taking a range of antiviral medications found no impact of those drugs on SARS-CoV-2 viral clearance rates.
A New York study found the number of intensive care patients on ventilators increased nearly 2.5-fold, and the median severity of illness increased 40-fold over just two weeks of the COVID-19 pandemic.
And while an earlier study suggested that higher levels of fine particulate air pollution were associated with higher COVID-19 mortality, another analysis of air pollution data shows significant declines in ground-level air pollution, which could decrease premature deaths and childhood asthma.
Finally, the ABC reported on an Adelaide numpty who recruited a team of people to stockpile around $10,000 worth of loo paper and hand sanitiser at the start of the pandemic has been refused a refund for his 132 packs of bog roll and 150 litres of hand sanitiser. We hope that puts a smile on your dial as you start the day. - Here are the latest infection figures around Australia, to 3pm yesterday:
National – 6,447 (up 47) and 63 deaths
ACT – 103
NSW – 2886
NT – 27
QLD – 999
SA – 433
TAS – 168
VIC – 1299
WA – 532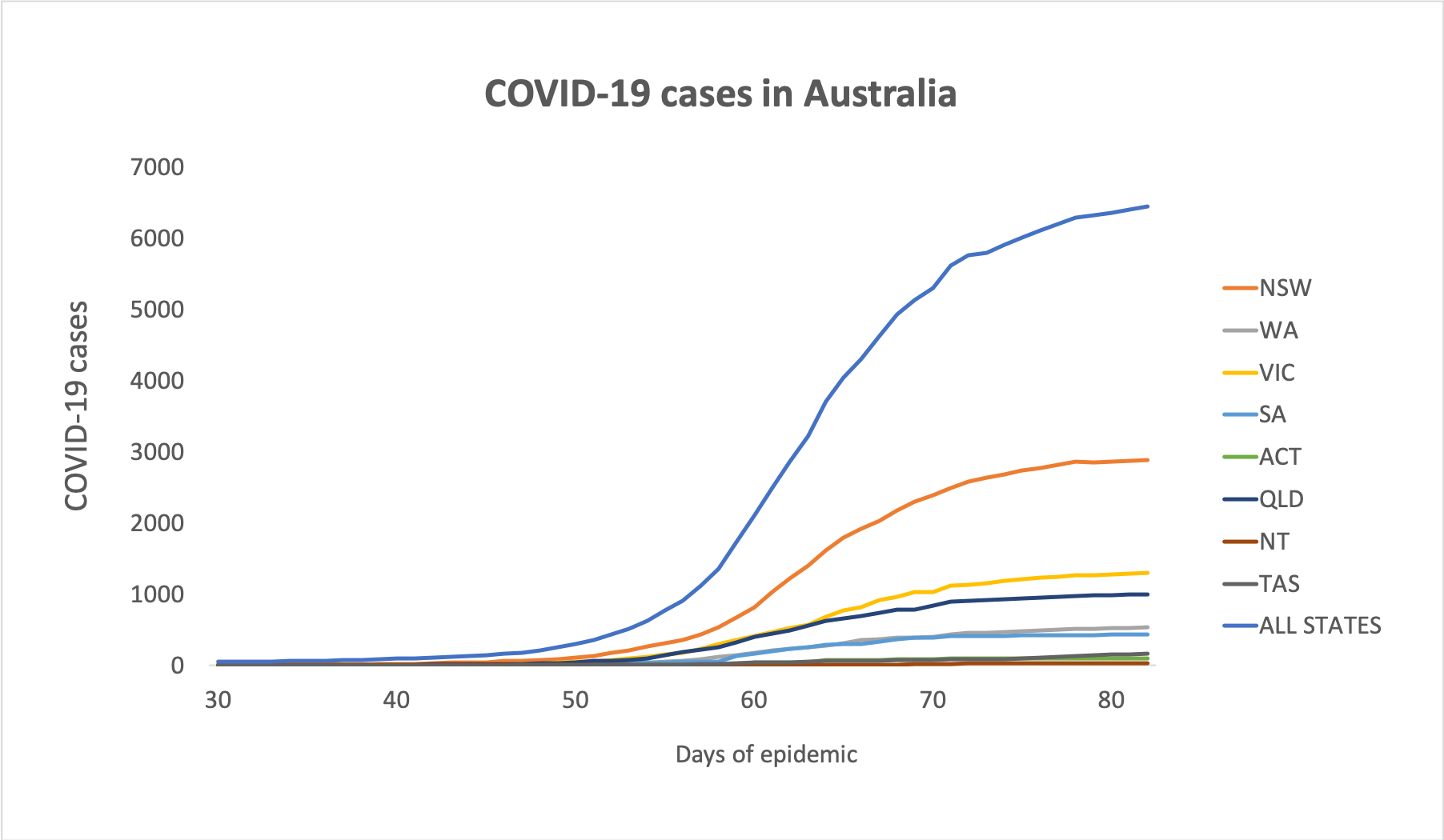
Disclaimer: The content on the Medical Republic COVID-19 blog is independently created by Medical Republic without input from Boehringer Ingelheim Pty Ltd. The views, information, or opinions expressed on the Medical Republic COVID-19 blog are Medical Republic’s own and do not necessarily represent those of Boehringer Ingelheim Pty Ltd. Boehringer Ingelheim Pty Ltd is not responsible for and does not verify the accuracy of any content on the Medical Republic COVID-19 blog.