After-hours providers have bungled how they have handled transparency around the growth of urgent items
After-hours providers have walked the GP community right to the front door of “looks like a duck, walks like a duck” with how they have handled transparency around the growth of urgent items.
But with last week’s MBS review we appear to have skipped straight to “it’s quacking, kill it”.
The review recommends that after-hours providers be denied access to urgent items, regardless of whether GPs were servicing patients or not. If implemented, it would go a long way to destroying an after-hours sector which the government had been trying to build back up for the last 10 years.
The key argument to kill off after-hours providers is that they have been rorting the system by over-servicing on urgent items. Adding to this, there is now research that strongly suggests the entry after-hours services into a region does nothing to decrease presentations to emergency departments (ED).
Just last week an article appeared on The Conversation website headed: “After-hours GP home visits strain the budget (and don’t help emergency departments)”.
The tone of the article was made clear the first sentence of the article: “After-hours home medical services are a burden on our health budget and don’t ease the strain emergency care, new research shows.”
That is not a trivial claim, nor is The Conversation a trivial publication. The website has a monthly direct audience of 3.5 million, and another 35 million through re-publication. It is very influential.
The same people who were writing the article had done the research, which had first been published in the peer-reviewed and evidence-based medical magazine, Australian Family Physician , an official publication of the RACGP.
We doubt there is a conspiracy here: that the RACGP’s official journal publishes an article purporting to reveal strong evidence that supports the views of the organisation’s leadership, expressed firmly to the highest levels of government in the lead up to the recent budget.
But the article, we think, is fundamentally flawed, and how it came about, and was received, says a lot about how emotionally charged and political the after-hours debate has become. And how careful we need to be in this debate.
The original piece of research appeared under the “research” section of the June issue of Australian Family Physician and was titled “Up, up and away: The growth of after-hours MBS claims”.
If the authors had left it at the headline they might have been OK. They present a retrospective analysis of after-hours items from 2011 to 2016 which shows the growth in after-hours items in the five-year period is quite dramatic in certain regions where after-hours medical deputising services had been introduced.
But this shouldn’t have been news to anyone. People are rightly worried that as the service grows, and awareness among the public becomes geographically more widespread, that drives the growth of urgent after-hours item numbers in areas where use had been relatively low.
The result, according to some, is a huge waste federal health money – most especially if, as is claimed in both the articles, the increase in use of these items puts no corresponding downwards pressure on ED presentations.
Growth in after-hours services has been spurred by a few things, some of which have been very deliberate on the part of the federal government, including:
• changes to item-number amounts and items to incentivise companies to expand the service –specifically, addition of urgent items
• changes to what category of doctors can perform after-hours services, so that the same companies have enough doctors to expand
The entry of private equity with a plan to roll up regional providers into one big national provider, and centralise systems and make money, was the icing on the growth cake. After hours, which had been dropping as a service for many years since a peak probably back in the 1970s, started growing again after 2010 – at first slowly, and in the last few years very rapidly.
As far back as 2004, former prime minister John Howard made, and then subsequently kept to a large degree, a number of promises to push after-hours medical services onto an around-the-clock basis, in order to service the community better. “Super clinics” were once meant to be part of the equation, but never quite fitted the bill.
Given the clear-cut nature of the MBS recommendations, you would expect that everyone would have some very clear evidence of what is going on. That we would know, for sure, the after-hours providers were rorting the system and that after-hours was having no effect on reducing ED presentations.
But where is that evidence?
When we spend nearly $300 million each year on after-hours urgent items, and we are all up in arms about what is happening, why haven’t we done any definitive research?
The Australian Family Physician article is one of the few actual dedicated pieces of research on the topic. It was well intentioned, but it was underfunded. It draws conclusions which it almost certainly can’t sustain because the methodology was wrong and the data was scant.
Here’s how it is likely wrong:
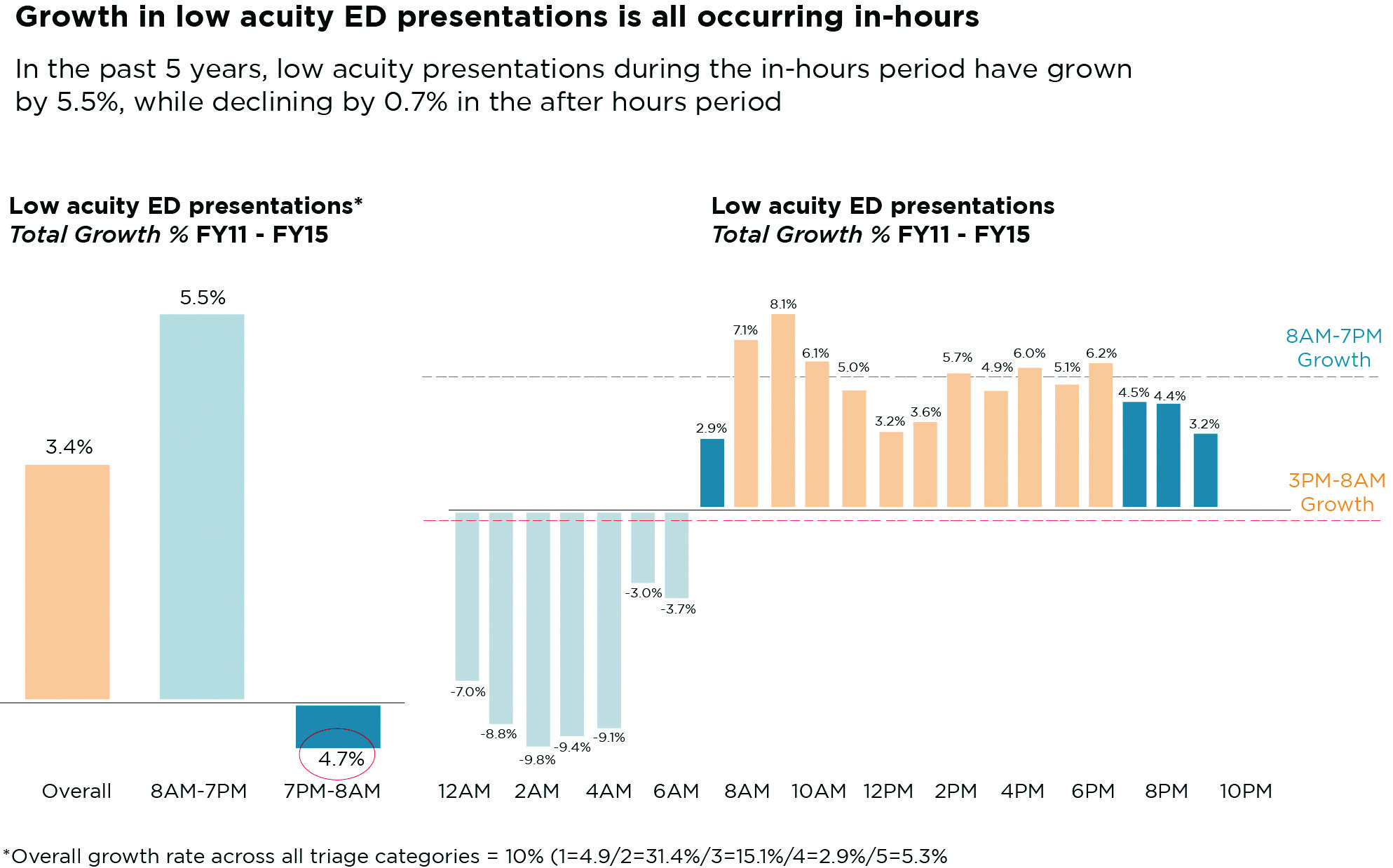
Comparing apples with apples and oranges: The paper compares averages of 24-hour presentations to emergency for low acuity presentations. But after hours isn’t operating on a 24-hour basis. You have to isolate the hours that after hours is operating and look at ED presentations for those periods. When you do that, you get an almost opposite picture to the results used to establish the conclusion that after hours is having no effect. That is, instead of a slight increase in after-hours presentations over the period there is actually a decrease. After hours starts at 6pm. From 7pm to 8am the drop in presentations is 4.7%. But if I were the after-hours providers, I would be pointing out that most of their calls come after 9pm, when people don’t have the option of going to an after-hours clinic. In this period, the drop is quite a bit more dramatic, at about 7.3 %. Given the overall increase is only 3.4% for the full 24-hour period, this might form the basis of a theory that after-hours services are working. But you can’t go there either, not yet anyway. What you can say, however, is that this paper has a very flawed methodology. It’s comparing apples, with the mean of apples and oranges, oranges being “in-hours” presentations to ED. (See chart 1, page 11)
A very important question to be asked here is: What is driving the growth of “in-hours” ED presentations? The answer might be as important as solving the after-hours data, in terms of saving money in the system.
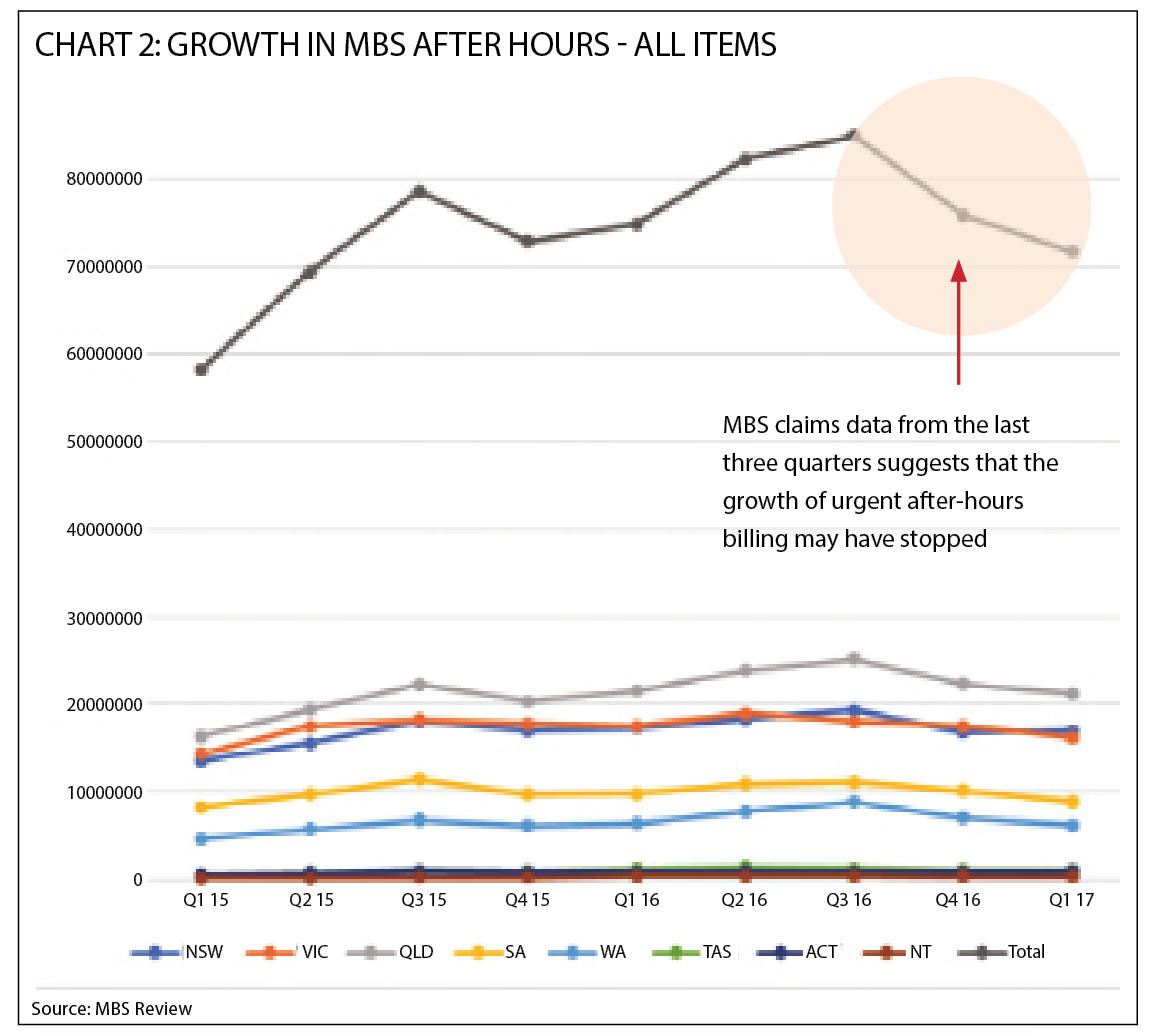
Not using up-to-date data: This may not be the researchers’ fault. It might be that, like many peer-reviewed journals, Australian Family Physician has glacial processes. Nonetheless, the data used to establish that after-hours services has been skyrocketing in the last few years stops at June 2016. It is interesting to check all the data available since, which we’ve done, and it uncovers something that might just be seminal to the after-hours story: all that growth seems to have come to a halt quite suddenly. (See chart 2, page 11).
If this trend continued, it would support an argument made by the after-hours companies that they have reached a saturation limit and won’t grow much more.
The National Association for Medical Deputising Services (NAMDS) providers say they predicted this would happen. If it does, what do we make of that?
Only using Tasmanian data: Not only did the study use average 24-hour presentation data to establish a pattern of ED presentation that was growing not shrinking, it used data only from Tasmanian public hospitals, not national data. National data for the period was available and available broken down by hour. It wasn’t used. That data shows a different picture.
No-one wants to believe a word that the after-hours providers say. The biggest provider, National Home Doctor Service, which has about 50% of the entire market, is run by private equity. Private equity is fundamentally disparate to the ideals espoused by most health-system professionals. Private equity just wants to make money. But should we be framing them with flawed studies and then assertions about their growth not scientifically calculated evidence.
It’s OK to be suspicious of these companies and their private-equity masters. For one thing, a lot of the advertising for these services seems to have disappeared in the last six months or so, at least in major metropolitan centres. Have the claims stopped growing because the services have hit a natural population saturation limit, as the after-hours providers claim? Or, have they deliberately slowed things down, by, for instance, reducing promotion, to take the heat out of sector and get some points back in Canberra?
The speed of the slowdown certainly feels suspicious. But we can’t make that call without robust evidence and data. If the providers are right and the doomsayers are wrong, we are destroying a sector that does a lot of good. The sector employs a lot of GPs, services about 50% of our GP practices and their patients, and has expanded into regional areas that couldn’t be managed by in-hours GP operations.
The biggest issue remains, no-one knows and no-one, probably rightly, trusts anyone.
We can’t get anywhere without robust research and data.
Why isn’t the government stepping in and sorting this out? Why not do a few controlled studies of regions where the NAMDS providers are establishing themselves versus ED presentations. Also, why not go into some of the bigger providers and do an external and independent audit of their urgent claims. If National Home Doctor Service said no to a request like that, you’d have a right to be suspicious and more grounds for breaking these services up.
The MBS review committee hasn’t got clear evidence. It is making assertions. Worse, they appear to have decided to change the definition of “urgent” items and retrospectively suggest that the definition has been misunderstood.
If it was misunderstood, why wasn’t something done a decade ago, when these providers first were granted access to the items? Are we really to believe that they’ve been doing it wrong for 10 years and no one did anything? Because the rate of claims per capita has not changed. What has changed is these organisations have created access to more of the population either by awareness campaigns or moving into new geographies where the service never existed. The way they classify “urgent” hasn’t suddenly been altered to make more money.
The somewhat ugly truth of why we are here is that there is not enough money to go around and something has to give. And if it’s between GPs, who have had their pay frozen for the last few years and a private equity owned corporation, the doctor fraternity, not surprisingly, is choosing for the GP community. That is not a problem with rorting. It is a problem with a government that has got it’s numbers wrong and simply will not spend anymore on health, so is forcing doctors to make a choice.
If it really is this choice, then opting for GPs first is possibly the right choice. But why is this an either or situation? Either way we are going to denude services to patients and to GP practices. Why are we being forced to the brink of potentially destroying the after hours infra-structure in a country where we have painstakenly and deliberately built that infra stucture up over the last 10 years.
No-one is saying things in after-hours are are moving along swimingly. No one is saying, don’t bother checking thoroughly what is going on in urgent items. But this has all the appearance of the government backing out of a commitment it made as far back as 2004 to Australian patients, and GPs, but very cleverly avoiding any scrutiny by reframing the situation in budget terms as you can’t have both a lift of the MBS freeze, and viable after-hours provision. They’ve pitched the RACGP against the after-hours providers using the growth of the urgent items as the catalyst for discontent and the MBS review committee has passed judgement without looking at the situation properly. After hours providers have somewhat foolishly walked into the government’s trap.
The explanation that the after-hours companies provide for the astronomical growth in urgent items is:
* the per capita rate of claiming has remained virtually unchanged
* the growth is coming from doctors seeing more of the population as these services move into unserviced geographies and make more people aware the service even exists
These arguments have a grounding in logic. As do the assertions of the MBS review committee, who say the growth is mainly due to over promotion of the services as “convenient”. But neither are proven.
And if we shrug our shoulders, as some GPs want to do now, and implement the MBS recommendations, then we risk destroying a service that 50% of GP practices use for their patients after hours, one which employs quite a few GPs, and one which even the RACGP admits is a critical training ground for GP registrars.
One GP responded to an online article we posted on this topic this way:
“I don’t think any of us will bemoan the loss of the after hours rort and convenience medicine … Anything that is an emergency they tell to call the ambulance … so the rest is just normal problems. It’s a further fragmentation of GP care. The money would be much better spent on day-time GPs.”
This isn’t an opinion or feeling that we should be ignoring. It feels like it sums up the view of a lot of GPs.
But is it really what our healthcare system architects had in mind when they opened up these urgent times a few years back and allowed these providers to use non GPs in order to find enough workforce to provide a wider range of service? We built these organisations up for a reason – better after-hours medical care, more access and reduced ED presentations.
Understanding the after-hours sector better, and managing it better, is surely a preferred route.
There are clearly issues to be sorted out because the money is tight. But are we happy to tear it all up having spent so much time and money building it up, for what is essentially, one possible crisis in over servicing?
The authors of the Australian Family Physician paper are one of very few research groups left in the country that are trying to get underneath the effectiveness of after-hours servicing and its relationship to ED presentations. How much would the Department of Health have to provide a group like this to find some concrete answers? They guess somewhere between $50,000 to $100,000.
In the last budget, the government gave pharmacies an additional $600 million for expanding community services and the Australian Digital Health Agency $375 million to expand the “opt-out” program on the My Health Record, which is something, so far, that is completely unproven.
Surely they can find $100,000 or so to resolve this very important patient and GP servicing issue.