It was a good idea at the time, but now it's holding us back.
Australia’s vaccine rollout has attracted significant criticism for its slow pace.
Around 13% of Australians have now received at least one vaccine dose, compared to, for example, 56% in the United Kingdom. We’ve heard reports of mass vaccine hubs in Melbourne sitting largely empty — though the current COVID outbreak has brought Victorians through the doors in record numbers.
There are a range of reasons Australia’s vaccine rollout is broadly lagging. At the core is the issue of vaccine hesitancy, in a large part due to the very rare blood clots associated with the AstraZeneca vaccine.
While addressing vaccine hesitancy will be key, as the Victorian outbreak shows, we should be looking at all possible strategies to boost our vaccine rollout. It’s pleasing to see Victorian hubs will now offer the Pfizer vaccine to people aged 40-49.
Victoria to enter a #COVID19 7-day lockdown from midnight as cases from Melbourne outbreak grows with 150 exposure sites. Vic Govt announces 40-49yr olds can get Pfizer vaccine from tomorrow. Getting vaccinated becomes 5th reason to leave home. #gettested https://t.co/S1mTLnzEE4
— Burnet Institute (@BurnetInstitute) May 27, 2021
Another way to speed things up would be to drop the phased approach to the vaccine rollout, and allow all Australians over 16 to come forward.
The rollout so far
At the outset, Australia’s vaccine rollout was broken up into phases to ensure those most vulnerable to being exposed to the virus and becoming very sick with COVID-19 would be prioritised.
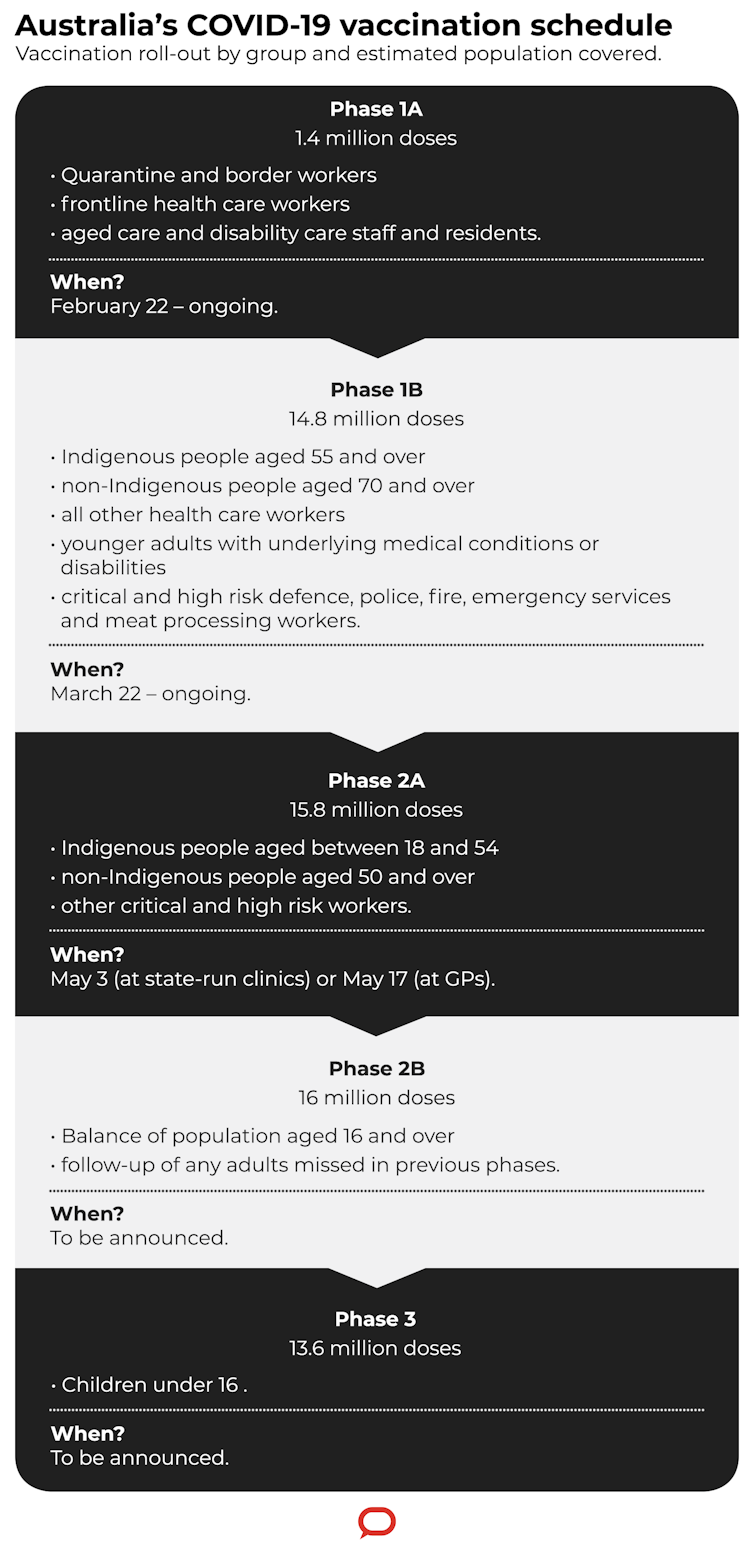
We’re now up to phase 2a which includes all adults over 50. Unfortunately, many people eligible under phase 1a and 1b are still waiting. It’s particularly worrying to see residents in aged and disability care who haven’t yet received one dose.
So when we consider the idea of opening up vaccine access more broadly, it is important this doesn’t compromise vaccinating priority groups. Another challenge will be working within vaccine supply constraints.
But there are good reasons to invite younger adults to be vaccinated sooner rather than later.
Targeting younger people
If younger adults become infected with COVID-19, they’re more likely than older adults to have mild or no symptoms and therefore be less infectious.
But it gets more complicated when you factor in behaviours and the fact an absence of symptoms means there’s no signal to practise precautions or to test and isolate.
Asymptomatic transmission is estimated to contribute to at least 50% of all infections.
Read more: 4 ways Australia’s COVID vaccine rollout has been bungled
If we also consider the generally greater level of mixing among younger adults in social and essential work settings, all of this together increases the contribution they make to the spread of the virus.
In Victoria’s second wave, adults in their 20s represented the highest number of cases.
So vaccinating younger adults is crucial for population-level protection, especially if the virus is circulating in the community.
Pfizer for under 50s
Bringing forward vaccination of those under 50 not eligible under phases 1a and 1b would place more demand on Pfizer supplies.
We’ve already seen the Northern Territory (outside Darwin) and regional South Australia take this approach, opening up the rollout to anyone aged over 16 in regional centres.
But Pfizer vaccines are a finite resource and the capacity for different states to do this is dependent on supply.
Recent changes to the shipping and storage requirements — the Therapeutic Goods Administration has ruled the Pfizer vaccine can be stored for up to one month in a normal fridge — will make distributing this vaccine a bit easier. Nonetheless, logistical problems remain.
We could convert some underutilised hubs to dedicated Pfizer hubs targeting younger adults. But we would need to manage demand within supply constraints, ensuring people aren’t turning up only to be told there are no vaccines available.
Victoria’s decision to bring forward phase 2b, but only for those 40-49, is one way to keep this manageable.
Read more: I’m over 50 and hesitant about the AstraZeneca COVID vaccine. Should I wait for Pfizer?
What about AstraZeneca?
Some experts are calling for under 50s to be allowed to choose to have AstraZeneca.
Under 50s are not currently prohibited from having AstraZeneca, but Pfizer is preferred. This guidance is based on the very small risk of adverse reactions to the vaccine balanced against the benefits of protection against serious illness or death from COVID-19.
The benefits outweigh the risks for over 50s. But as you get into the younger age groups the gap between the benefits and risks narrows with their lower susceptibility to severe COVID-19.
This latest outbreak in Victoria shifts the equation somewhat. But I don’t think we’ve reached a point yet where we should throw away existing guidance and recommend the AstraZeneca vaccine for younger people.
If a younger person turns up to a vaccination centre and says they’d like to receive the AstraZeneca vaccine, that’s a personal choice. But if we’re going to expand the AstraZeneca rollout to under 50s, we would need to ensure we have the information, consent and accessibility completely worked out so it’s an informed choice.
Getting it done
The phased approach was the right idea at the start. But now, with complexities such as vaccine hesitancy and distribution challenges, this approach is holding us back. While not taking our attention off the urgent need for aged care and disability care residents to be vaccinated, I argue it’s time for a rethink.
Though information about vaccine supply is not entirely clear, there probably aren’t enough Pfizer doses to offer 16-49-year-olds across the country. Victoria’s decision to prioritise 40-49-year-olds is a good compromise, recognising this group stands to benefit the most of those under 50.
We likely do have enough AstraZeneca to offer it to people under 50 who want it, as long as we ensure the right checks and balances are in place.
We also might benefit from exploring other ways to improve vaccine coverage, such as shortening the interval between doses, or trying to cover more people with just one dose, or even mixing and matching different vaccines.
Read more: From faith leaders to office workers: 5 ways we can all be COVID vaccine champions
Once supply moves ahead of demand, we must have processes in place that make efficient use of our vaccine resources and facilities, minimise vaccine wastage, and ensure our population vaccine coverage builds quickly.
We want all Australians to have the chance to be vaccinated, and we should continue to prioritise those who have the most to gain. But we shouldn’t let vaccine hesitancy set the pace for our entire campaign and allow vaccine hubs to sit idle.
Catherine Bennett, chair in epidemiology, Deakin University
This article was originally published at The Conversation


