Years of research are finally translating into practical treatments for severe asthmatics that are offering genuine hope
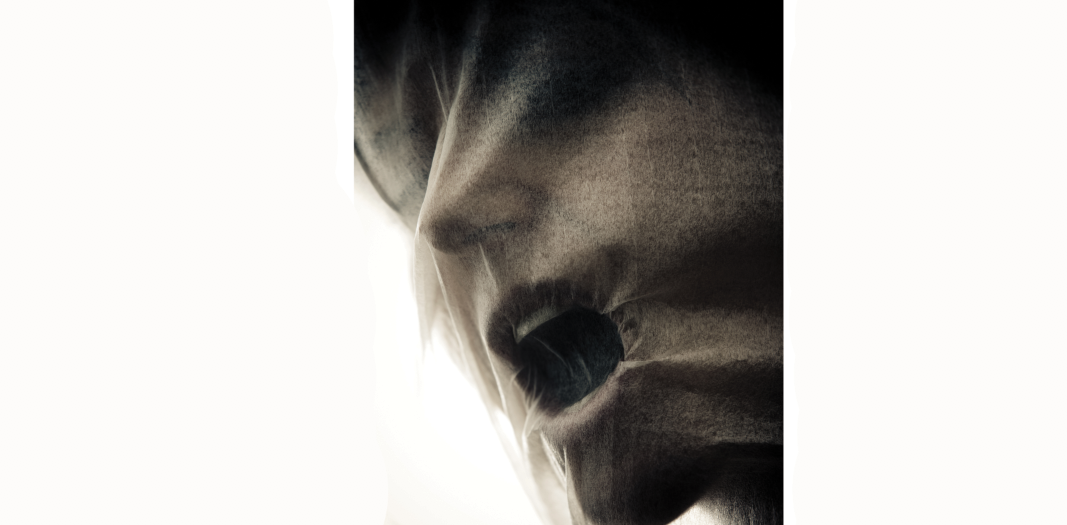
While her husband and daughter climbed the tower of Pisa, Mystie Gazzola couldn’t even walk up an alleyway.
Her lips were always blue, she had to use disabled parking, she was constantly in and out of hospital, and she didn’t think she’d make it to her 40th birthday.
That was before mepolizumab, one of the monoclonal antibodies (mabs) that is changing the lives of severe asthmatics. While only 5-10% of people with asthma have it badly enough to qualify, this still represents up to 200,000 Australians – and more mabs are on the way.
“I’ve been healthy as a horse,” the 39-year-old says of her 16 months on the biologic. “I don’t even say I have asthma any more. The dark rings under my eyes are gone, my lips are a pinky colour. I’m going to the gym – I’ll probably outlive everyone!”
Having spent decades doing the “puffer shuffle” and taking buckets of prednisone – 50mg a day towards the end – Gazzola has had her life transformed by this IL-5 inhibitor. So why did it take her so long to find a doctor who’d prescribe it, when it’s been on the market for several years?
Her respiratory physician/knight in shining armour, Dr Greg Katsoulotos, says while the drugs are “horribly expensive”, they are well worth it for the public health dollars they save on hospital and ICU visits and the health complications brought about by prolonged oral steroid use: osteoporosis, hypertension, skin problems, weight gain and diabetes.
“There is a threshold for oral steroids in your life above which you’re probably going to be left with permanent long-term complications, and the reality is if you have two or three courses of high-dose prednisone you’ve probably reached that maximum,” he says.
“These antibodies target one part of the immune system, rather than steroids which are like a machinegun with lots of collateral damage. With these very specific targeted treatments you achieve much better asthma control, fewer symptoms, fewer attacks, and much less oral steroid usage with less side-effects.”
He says a small group of “believers” prescribe the IL-5-targeting mepolizumab (Nucala) and benralizumab (Fasenra) for severe eosinophilic asthma, and IgE-targeting omalizumab (Xolair) for severe allergic asthma, while some prescribe them occasionally and others not at all.
That’s not hard to understand, given the work required to ensure the diagnosis is correct and criteria for severity are met, and the ongoing reviews required by the PBS – which in turn are justified, given the $20,000-$30,000/year cost of these drugs.
“I’ve honestly had referrals from other physicians to do the application,” Dr Katsoulotos says. “It’s just a few pages of a PBS form, it’s a bit messy and takes a bit of organising, but it becomes second nature.
“There’s lots of reasons why people don’t use them. But when people have had a good response they keep going.”
The mabs have to be prescribed by a respiratory physician, clinical immunologist, allergist or general physician experienced in the management of patients with severe asthma – not by a GP. Presently the once or twice monthly injections are given by a doctor or nurse, but companies are working towards having auto-injectors approved.
Connie Katelaris AM, Professor of Immunology and Allergy at Western Sydney University, was involved in the trials that led to the registration of omalizumab and has continued to run trials at Campbelltown Hospital in Sydney’s south west.
Next out of the pipeline will be dupilumab, which targets IL-4 and IL-13, and tezepelumab, which targets the TSLP molecule right at the start of the inflammatory cascade. Tezepelumab should be effective for not only high but also low eosinophilic asthma.
“That’s still in trial, but the concept is exciting as it’s a little different,” Professor Katelaris tells The Medical Republic.
“Over the past 20 years there’s been a huge amount of research that’s helped us understand mechanisms and pathophysiology, and what we’re seeing now is the translation of that knowledge into actual practical treatments that are targeted to the molecules we think are key in asthma.
“It’s an exciting time to be treating patients with severe asthma: finally we’ve got something that’s really terrific to offer them that brings about a huge improvement in quality of life and lessens their exposure to steroids and all the attendant problems that those treatments have.”
The three monoclonals currently on the market, all made by different pharmaceutical companies, “work remarkably well when the patient is correctly chosen”, she says.
“The majority can be controlled on much simpler, cheaper medications. We’re only talking about 5 to 7% who have exacerbations, who end up in hospital, who have oral corticosteroid treatment, who have optimal inhaled medication but are still not controlled and are highly symptomatic.
“In that group these monoclonals are a godsend, they have transformed lives. But these medications are incredibly expensive, they are ongoing treatment, so people have to be on these for years. We know that if you stop them there’s a gradual deterioration. So we know that these control, they don’t cure, they’re not disease-modifying.”
While it’s only the worst cases who’d be on 50mg of prednisone a day, Professor Katelaris says, there are plenty more who could benefit from the monoclonals’ steroid-sparing effect.
“They are a real bonus, they’ve opened up more sane management for this group and it’s sparing them steroid side-effects. Not many would be on daily 50, but many would be on 5, 10, 20mg a day long term, and that has its consequences in osteoporosis, obesity, hypertension, diabetes and all the other nasty side-effects. Weighed against that, this becomes very feasible and I’d say cost-effective, to keep patients out of hospital and minimise all those comorbidities.
“Any patient with severe asthma requiring frequent oral steroids for control should be sent along to immunologists or respiratory physicians with an interest in this to be evaluated for the feasibility to step up to one of these newer treatments.”
Dr Katsoulotos, who has about 50 patients on the monoclonals, says they are well tolerated, with the commonest reaction being some redness at the injection site. He says omalizumab has good safety data and the others are still in long-term studies with a good safety signal so far.
He says measures of lung function should be part of general health checks.
“They do cholesterol, why not basic spirometry testing? To pick up that someone has low lung function early on would be a huge thing: you may be able to turn it around, rather than wait for years till you have a lung you can’t repair easily.”
Professor Katelaris says the inhibitory effect of the PBS requirements is necessary to ensure only the right patients are given the drugs.
“If you’re talking about medications that cost $20,000 to $30,000 a year ongoing, you do need gatekeeping. GPs aren’t able to prescribe these, but they should be identifying patients who need referral.
“It’s onerous, but it’s life-changing therapy. A couple of things could be tweaked – repeat prescriptions could be made a little easier – but the idea is that patients are reviewed at regular intervals to ensure they’re still gaining benefit. Yes, it adds to our workload, but the rewards are immense.”
Gazzola would agree.
She first met Dr Katsoulotos the day after being discharged from hospital after a two-week stay. He took one look at her and said she needed to be in hospital.
“I’d followed every asthma management plan put in front of me – because you want to breathe, you want to live,” she says. “They ran out of puffers for me to try. Every new doctor would say try this puffer and add some prednisone. I didn’t think I was going to make 40. I was getting sicker and sicker, waking up gasping for air.
“Dr K. was the first doctor who didn’t say puffers and prednisone, he said there’s so much more out there. He did all the lung function tests and blood tests and got a baseline and said this is the way we’re going to go.”
It was one week before she noticed the difference.
“Since I’ve been on Nucala I haven’t touched prednisone or a Ventolin puffer. I don’t even carry one any more, which makes Dr K. cringe.
“I can guarantee I wouldn’t be here if it wasn’t for Dr K. He can’t retire.”