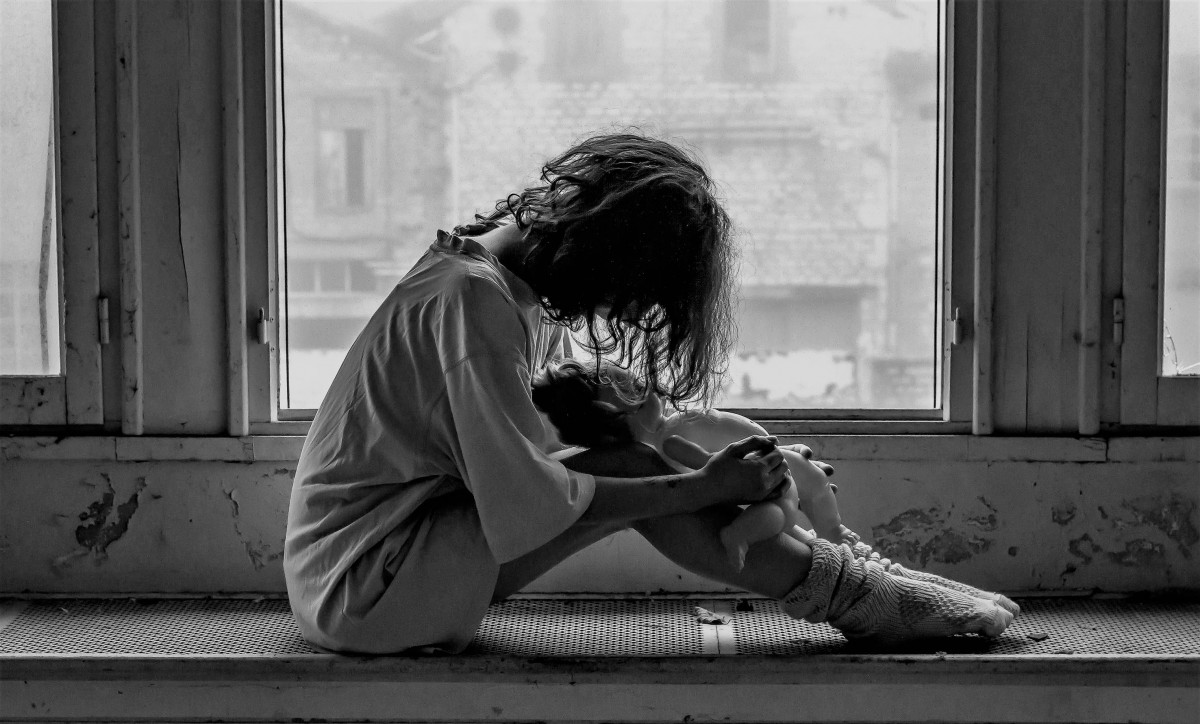
Girls, younger children and families from non-English-speaking backgrounds are the least likely to access mental health services, research shows
Three-quarters of Australian children with mental health disorders aren’t getting professional help, according to new research.
Girls, younger children and families from non-English-speaking backgrounds are the least likely to access mental health services.
We looked at the mental health of just under 5,000 Australian children aged eight to 13 via parental surveys of their child’s emotional and mental health. We then linked the results with Medicare data to see which families had accessed help.
Fewer than one in four children we identified as having a mental health problem saw a health professional in the 18 months after we surveyed them.
Left unaddressed, mental health problems can become more entrenched and harder to treat. And mental health problems in childhood can have lifelong ramifications including increased risk of mental health problems in adulthood, poor educational attainment, unemployment, and contact with the criminal justice system.
So ensuring children and adolescents who experience mental health problems receive access to timely and effective care is essential.
What types of mental health problems do kids have?
Around 14% of children and adolescents aged four to 17 meet diagnostic criteria for at least one mental health disorder.
The most common mental health disorders in Australian children in this age group are anxiety disorders, which affect 6.9% of children, and attention deficit hyperactivity disorder (ADHD), which affects 7.4% of children.
Around 50% of all adult mental disorders begin before the age of 14. Yet in 2017-18, children under the age of 15 had the lowest use of Medicare-rebated mental health services (5.1%) of any Australian age group.
Younger children
Younger children were less likely to access services than older children. Some 20-27% of children aged 12-13 years accessed services, compared to 9-15% of children aged eight to nine years.
Young children respond to and process emotional experiences and traumatic events in ways that are very different from adults and older children. Consequently, it can be more difficult to recognise problems in early childhood.
A child acting up in the classroom, for example, may be perceived as being “naughty” rather than having mental health problems. Or a child may experience stomach aches and headaches which are caused by anxiety but thought to be a physical problem.
When problems are recognised, families may delay getting help for young children in the hope that they will “grow out of” the mental disorder.
While this may apply in some cases, treatment is still important. Take ADHD, for example. Although about 80% of children with ADHD will grow out of it by adulthood, children with ADHD often find it hard to make friends. If they miss out on developing their social skills early in life, it can become increasingly difficult to make friends during adolescence and adulthood when peer relationships become more complex.
In our study, the factors most consistently associated with getting support were symptom severity and parent perception that the child needed help.
The gradual onset and increase in severity over time of many mental health problems means children and their parents are more likely to seek services when the symptoms become severe or impact significantly on the child’s ability to function. This typically occurs as they grow older.
Read more: Children’s well-being goes hand in hand with their dads’ mental health
Boys versus girls
We found girls were less likely to receive care than boys. Girls made up 50% of children with mental health problems in the study, yet accounted for just 30% of children who received support for emotional problems at ages eight to 11.
This may have something to do with the fact that mental health conditions can be more difficult to recognise in girls.
Boys are more likely to externalise problems such as anxiety by reacting angrily when asked to do something that upsets them. Girls are more likely to internalise these issues by withdrawing or appearing very quiet, making problems harder to detect. In an environment like the classroom, boys’ problems are more likely to get noticed because of their disruptive nature.
Culturally and linguistically diverse backgrounds
Around 14% of children with emotional problems came from a non-English speaking background, but they only accounted for 2% who received help.
The reluctance of parents from non-English speaking backgrounds to get help may be related to different cultural understandings of mental health and illness. They may also struggle to find services for their child in their own language.
Mental health conditions may also be more difficult to recognise among children from non-English speaking backgrounds, where quietness in the classroom may be mistaken for a language issue rather than a mental health issue.
We need change
Over the past 20 years there has been little change in the prevalence of child and adolescent mental disorders in Australia despite increased investment in resources. This is likely in part because the quality and the intensity of services provided have not improved.
Children may not be receiving sufficient treatment sessions or treatment sustained over a long enough period to meaningfully impact on their symptoms. It’s recommended that children receive at least eight sessions of cognitive behavioural therapy for the treatment of anxiety, for example, but many children will require more.
Australia’s health system rewards discharging patients from care within a set number of appointments rather than once they have improved. The Medicare Better Access scheme allows for a maximum of ten subsidised appointments with a psychologist in a calendar year. But again, many children require more.
Read more: What about the mental health of kids with intellectual disability?
We need a system-level shift to funding based on measured symptom improvement rather than a capped number of appointments both in hospital settings and in the community.
Our research suggests we need to better understand parent and child drivers of why children miss out on care, particularly girls, younger children, and those from diverse backgrounds. Doing so and ensuring access to high-quality care will benefit not only the child and their family now but also the adult they will become.
Authors
is Postdoctoral research fellow, Murdoch Children’s Research Institute
![]() is Principal Fellow, Department of Paediatrics, The University of Melbourne, Murdoch Children’s Research Institute
is Principal Fellow, Department of Paediatrics, The University of Melbourne, Murdoch Children’s Research Institute