It’s a clever budget that offers hope and has doctor groups laying down arms but commits nothing to much-needed systemic reform.
My favourite assessment of the budget this week came from a local English journo in the media sector who once attended budget lockups in that country. His take came from one of his lockup friends who often would frame a new budget to his fellow journos as:
“Nothing to start a riot, nothing to stop a riot.”
In terms of the where the GP sector has been heading for the past few years, revolution and riot has certainly been brewing and this budget is at least an acknowledgement that the government sees that.
Dr Karen Price pretty much started the riot ball rolling in the last year of her presidency of the RACGP when she publicly proclaimed that GPs had nowhere to go but to abandon bulk billing.
The government had to do something to stop the place starting to look like late 18th-century France.
They did just enough to “stop a riot”.
They also seem to have done enough to have GPs all over the country a bit confused as to where they stand now.
Is this the beginning of a new era for GPs, or not?
It’s impossible to tell, of course.
The government has cleverly done enough to provide the AMA and the RACGP with the ammunition to take some credit for all their hard lobbying work in the past few years and suggest victory is nigh, but to simultaneously have GPs all over the country debating whether they think this is a new beginning or not.
If the natives are revolting, a great tactic is to confuse them by lobbing enough goodies over the fence to get them to start debating among themselves the value of the goodies.
Here’s one interesting take from Dr Imaan Joshi on the situation.
She spent quite a bit of time poring over social media posts to try to understand what was going on in the collective GP mind all over the country.
Dr Joshi is one commentator who isn’t at all convinced of what the RACGP tried to sell to its members this week in its this budget is a “game changer” press release.
Here’s a bit of the RACGP press release to give you some flavour:
The Royal Australian College of GPs (RACGP) has welcomed the federal Budget as a game changer for GPs, practice teams and the patients they care for across Australia.
RACGP President Dr Nicole Higgins said the Budget is a win for patients.
“Every patient deserves access to high-quality, affordable and accessible general practice care, irrespective of their postcode or income,” she said.
“I commend the Albanese Government for committing to this massive investment in general practice care. We know the problems impacting our health system can’t all be fixed in one go, but tonight’s Budget includes a ground breaking investment in the health of all Australians by strengthening general practice care. The Government has shown real commitment to strengthening Medicare and rebuilding general practice care for all patients.”
Dr Higgins said the $5.7 billion funding package in the 2023-24 Budget responds to calls made by the RACGP.
This release and similar sentiments coming out of the AMA might point to a real danger in this budget for a GP sector that was just starting to get its mojo on.
Firstly, the budget does send some good signals, and GPs and their member organisations would not be doing anyone any favours if they came out and proclaimed this was bad budget given the dire circumstances GP find themselves in.
But this budget is not by any stretch of the imagination a “game changer” for GPs and their patients.
No, this budget is more “placeholder to avoid rioting in the short term, and keep watching this space to see how serious the government might actually be”.
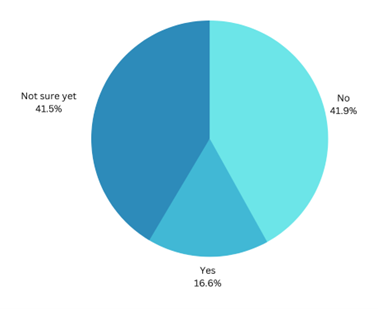
We did a pulse check via a flash survey and it looks like GPs seem to be leaning to the placeholder view, rather than the game changer view (the sample size is about 220).
But you can see from how big the “not sure yet” piece of pie is how confused everyone seems to be.
Q: Do you agree with the RACGP president that the budget is a “game-changer for GPs, practice teams and patients”?
In the same survey we asked whether the budget might change bulk billing behaviour and the result was a lot more black and white.
Q: Will you bulk bill more patients given the tripling of the incentive?
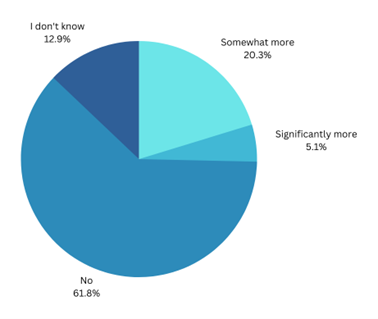
If the results of this question turn out to be representative (it follows a lot of anecdotal comments we’ve seen on social media) then we surely have a “we are not in Kansas any more” moment for the government, the profession and the healthcare system.
The tripling of the bulk billing incentive, which took the lion’s share of the overall dollar commitment in the budget at $3.5 billion, hasn’t moved the dial meaningfully on GP behaviour by the look of things.
If it’s true, it looks like we aren’t ever going back to the idea of a free universal healthcare system.
Which under the circumstances might be a practical way to view things now.
The bulking billing changes should help a lot in the country, and help somewhat those postcodes in cities and towns where patients simply can’t afford to pay a gap fee.
But here’s the big problem with stuff like this in a budget that isn’t addressing systemic reform issues.
One systemic reform issue is workforce.
The government might say that significantly upping the bulk billing incentive rate in the country for a large proportion of the patient population is addressing the workforce crisis in the country.
But it’s not.
One big problem with increasing the rate is that in many rural and remote regions there simply aren’t any GPs any more that can take advantage of it on behalf of any patients out there.
As an example, it almost certainly too little too late for Mildura, which lost its only bulk-billing practice when Tristar went under a year ago, exposing more than 13,000 of its patients to the harsher realities of have to front up to mixed billing practices only.
While some of the remaining mixed billing practices in the town might see the new incentive as enough to return a few of these ex Tristar patients to free care, it’s never going to be the same in that town again.
One really good question asked across social media this week was whether this budget would be enough to reverse the downward spiral of trainee doctors choosing not to take the path of becoming a GP.
Mostly people said probably not.
There are plans for workforce reform, but they are loose and eclectic.
There is no overarching plan from the government to go from A to B on whole health system reform where you could put such plans in meaningful context.
And this is very apparent in the budget.
Two examples of big budget items which promise such system reform but for which there is no evidence that any plans exist which will lead to it are My Health Record and voluntary patient enrolment, now rebranded MyMedicare.
The next big ticket item in this budget as far as Medicare and reform is concerned is the $950m for digital health.
About half of this $950m is to keep persisting with the My Health Record, and most of the rest is to keep persisting with the Australian Digital Health Agency, which came up with the My Health Record and has so far spent over $2.2 billion on it with nothing much to show for that spend.
Health Minister Mark Butler gave the My Health Record such a bollocking prior to the budget that everyone expected some big changes to how this project was run and where it was heading.
But the budget revealed that in fact the government is changing virtually nothing with this project. The only change is we are going to spend a lot more ($429m), yet again trying to make the My Health Record model work somehow.
If you’re a GP it would be hard to comprehend (or care about) just how much continually screwing this part of health reform up has impacted you already and will continue to do so in the future.
It’s all technical stuff and grandiose theory that must feel like it has nothing to do with day to day survival as a GP, but enabling our healthcare system to share meaningful data in real time between providers and with patients is possibly the most fundamental reform the government can pursue to help reinvent the GP sector as a the future hub of community and outcomes-based care.
But if we do what the budget is saying we are going to do, that is not going to happen.
If you’re interested in the gritty detail of why, you can read that here in our sister publication Wild Health.
The long and the short of it is that My Health Record is technology that all the successful reforming countries overseas abandoned quite a few years ago for its shortcomings, but for some reason we are happy to keep pouring money into it.
If we don’t change how we approach setting up infrastructure in our healthcare system that can share meaningful data seamlessly in real time, then GPs are going to be trapped in their old business model, unable to set up effective networked community care teams, unable to talk to allied care or hospitals, unable to compete with rapidly emerging and cynical online care model providers like Pilot and Mosh, and unable to integrate meaningfully with their local hospital network so they can truly be in a continuum of care that might shift the dial on chronic care management.
As much as no one will look at this aspect of our spend in this budget because digital health has always been hard to understand and no one has ever seen much practical come out of it (not completely true as our e-script network shows us some of that potential), it’s a vital piece of reform that the government still seems to have not got its head around.
VPE or MyMedicare is another good example of near meaningless promised reform.
Nowhere is there any detail available on why we going to spend upwards of $90m piloting this concept and how it might actually deliver anything meaningful to patients or the sector.
There are big picture statements about why we are doing it: the most banal is “so patients can be closer to their GP in their longitudinal management of care”.
But if you dig beneath the big picture statements statement VPE might be better described as vapour patient engagement which could easily end up wasting GP time and money.
There are fundamental problems with the idea that no one is addressing so far:
- What’s in it for a patient to bother to enrol, especially that very large cohort of patients who already think that their main GP is and always will be their GP?
- Even if a GP enrols a patient, what changes in their technology set up that would enable them to manage said patient in the manner the big picture statements are saying they will be? Answer, none. GPs current patient management systems aren’t designed to capture and management patients in the manner being proposed (in fact the enrolment work is all via an outside government system which no one has seen yet), and they aren’t designed to understand patient data and feed it back well enough to a GP to manage the patient significantly better longitudinally. Most importantly they aren’t designed to capture data that could measure outcomes so the government could fund the VPE system based on actual outcomes.
- A lot of the money so far is not being directed at GPs but at the PHNs to decide which patients a GP should enrol in this system. A lot of PHNs aren’t well managed enough to pull this off and some are completely disconnected from large sections of their local GP population, so how is that going to work and be fair?
- No one has any idea if the time taken to enrol and manage a patient in this system will provide an ROI to a practice to participate. This is a key reason why Health Care Homes failed.
When you subtract the bulk billing incentive, digital health and VPE, there isn’t much left and what is left is scattered about a bit aimlessly, as if there was last minute ticking of some boxes to make as many people happy as possible, such as in the case of increasing workforce incentive payments, but only by a long way short CPI, which is pretty meaningless.
Not withstanding all this, the RACGP seems to have stretched its imagination enough to believe that what feels clearly like “placeholder” actually marks the start of a journey to “game changing”.
Politically that might be a sensible position to adopt.
Practically, if they really go into some sort of “our work is done here” mode, we’re likely to be in a lot of trouble here.
If you break down the component parts of what is on offer in this budget there is nothing at all that addresses the sort of long term systemic reform that will be needed to secure the future of the GP sector, the health system overall and therefore patients.


