Advances in technology mean improvements in surgical techniques continue apace.
The technology in spine surgery has been developing at a rapid pace since the 1980s – and it is showing no sign of slowing down.
Current technologies surgeons take for granted include MRI scans, intraoperative CT scans and real-time neurophysiological monitoring of the spinal cord and motor function during scoliosis surgeries.
However, navigating the anatomy of the spine has always been a challenge, and even with two-dimensional imaging, such as X-rays and image intensifiers, inserting implants in the spine is a skill that requires many hours of training.
The development of intraoperative CT scans has enabled surgeons to “navigate” around the spine much like driving a car with a GPS.
However, the limitation is that the repeated use of intraoperative X-rays poses a danger to both the patient and staff in the operating theatre.
7D technology
A new image guidance system allows the surgeon to better visualise a patient’s anatomy by giving them visibility of where tracked surgical instruments are positioned in relation to three-dimensional and cross-sectional images of the spine.
7D Surgical’s machine-vision technology, which uses a 7D system, makes use of visible light reflected back from the anatomy and registers the image with a pre-operative CT scan.
Machine-vision technology is similar to that of self-driving cars, using special cameras to quickly analyse the surface of the spine. The system then uses this data to digitally register the patient’s operative position with a pre-operative scan, creating a real-time 3D image of the patient’s anatomy within seconds. The 7D system enables the surgeon to rapidly position tracked surgical instruments with accuracy, precision and zero intra-operative radiation.
Robotics
With more reliable navigation technology, surgeons are now able to add robotics to their operating theatres, adding further accuracy to spinal instrumentation.
Instrumentation of the spine adds stability to the spine segments as surgeons seek to correct deformity and re-align the spine. This practice was a technological breakthrough in the 1960s, allowing spinal fusion to be much more successful because the stability instrumentation adds to the segments to be fused.
Pedicle screws were first used in the 1980s. The technique was initially perfected with the free-hand approach and then by using 2D X-rays and image intensifiers. Now, CT and 7D technology have greatly enhanced the accuracy and decreased the morbidity that misplaced screws can cause. In addition to navigation, robotic spine surgery has added a further level of accuracy in screw placement, especially in minimally invasive spine procedures and in patients with challenging anatomy.
Robotic spine surgery uses a computer-guided mechanical “arm” to present the trajectory the surgeon has chosen during the planning of the instrumentation. The “arm” typically holds an instrument, such as a drill guide, to point the correct trajectory for the surgeon to drill and place the pedicle screw. Robotics has been widely used in orthopaedic surgery to aid surgeons in making the correct bone resections in knee replacements and helps pelvic surgeons access hard-to-reach anatomy in the depths of the pelvis to remove tumours and aid in visualisation.
The main drawback at present is the cost of robotic technologies, which are two-to-three times the price of image-guided systems, adding to the overall burden of costs on the healthcare system. However, cost-benefit analysis shows that in high-risk surgeries, preventing implant complications can more than offset these costs in some surgical areas.
Endoscopic spine surgery
The first human knee joint was arthroscopically examined in 1950. Watanabe, Takeda and Ikeuchi published their experience with 300 patients in the Atlas of Arthroscopy in 1957. Since then, the arthroscope has been widely used by orthopaedic surgeons in other synovial joints and general surgeons in the abdominal cavity, in a procedure called endoscopy.
In the early days, the visualisation of the anatomy was directly through the cannula. Since the development of charge-coupled device cameras (capable of converting light input into electronic signals) the technique became more akin to the procedure we know today. With further development of camera, lighting and video displays, the technique known as endoscopy (“endos” is Greek for “within”, “skopein” is “to observe or view”) has developed exponentially in the past few decades.
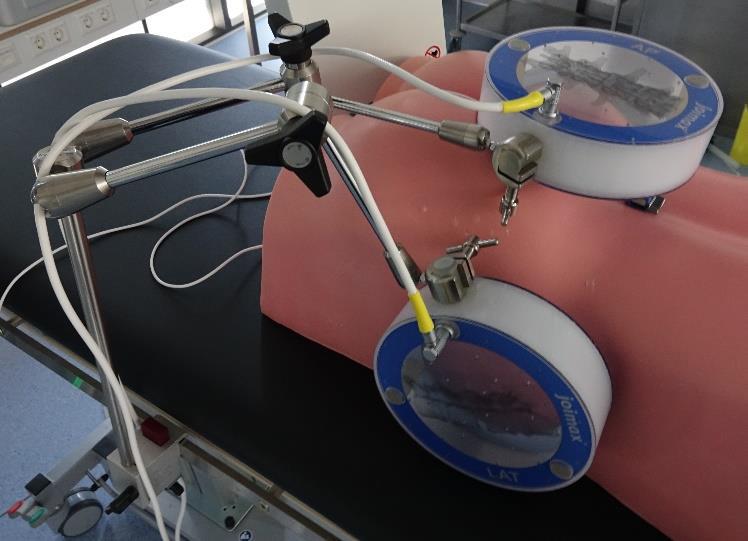
The spinal canal is not an enclosed cavity like the knee joint or abdominal cavity, therefore fluid flow into the area has to be carefully managed. Irrigation with fluid aids visualisation of the structures with the endoscope and helps remove blood and debris from the visual field. An increase of the fluid pressure in the surgical site can cause pressure on the neural structures, causing symptoms. Modern fluid-pressure monitoring systems gives the surgeon more control and an added level of safety.
Modern navigation technology allows the surgeon to visualise the position of the endoscopic instruments as they are placed in the patient’s body, adding to patient safety and reducing radiation exposure to the patient and surgical personnel. Using this technology, interbody cages and pedicle screws can now be placed as well in these Endoscopic Lumbar Interbody Fusion (Endo-LIF) procedures.
The technique allows minimally invasive decompression and/or fusion of the spine for faster recovery and a shorter hospital stay.
Magnetic growing rods and vertebral body tethering
The treatment of scoliosis has evolved and been refined over many years. Bracing dates back centuries but has been more carefully documented since the 1950s. Recent large clinical trials have again affirmed the place for bracing in treatment of adolescent idiopathic scoliosis in the growing child.
Two more recent advances in scoliosis are magnetic growing rods and vertebral body tethering.
In young patients who develop scoliosis, bracing is sometimes unable to control the progression of the curve. This can lead to severe deformity that can lead to severe restriction of lung capacity and can in rare cases cause death due to cor pulmonale (curves >100°).
Spinal fusion, while useful in arresting the curve progression, leaves the child with a shortened trunk and severe restriction of respiratory capacity. It is therefore desirable to delay spinal fusions for scoliosis as long as possible, provided the curve can be controlled adequately.
The so-called growing rod refers to a spinal construct where only one or two levels are instrumented and fused while the rest of the spine is allowed to continue to “grow”. In the past this required repeated trips to surgery where the rods were manually lengthened while the patient grows. Wound complications were common with repeat surgeries.
With the invention of magnetic driven rods, an electromagnet is used close to the patient’s skin and implanted magnetic rods allowing surgeons to activate the internal mechanism that lengthens the rods without surgically opening the wound. This is painless, takes about 60 seconds and can be repeated as often as necessary to match the child’s growth rate. This has been a revelation in avoiding repeat surgeries in young children along with the psychological effects of hospitalisations.
Vertebral body tethering (VBT) is a technique that is still under evaluation and its indications are being refined every three to six months. This technique places a compressive force over the convex side of the spine to permit the concave side of the spine to grow and create a straighter spine. This is a type of growth modulation technique not dissimilar to surgeries for leg lengthening and angulation correction procedures in orthopaedics of the growing child.
As mentioned above, spinal fusion has had many advancements over the years – it does reduce the motion segments in the spine and results in less spinal mobility. The desire to maintain motion in the spine has led to the trial of this technique, which was first reported in human subjects in 2010.
VBT is a thoracoscopic, minimally invasive technique in which screws are placed into the vertebral bodies on the convex side of the coronal deformity. The screws are placed into the middle of the vertebral body with bicortical purchase under fluoroscopic guidance. A high-strength, braided polypropylene tether is then placed into the screw heads and sequentially secured to each screw after segmental compression. The technique achieves modest correction of the spinal deformity immediately after surgery.
We do not have long-term studies on this technique yet. We simply do not know what the consequences are of tether breakage, the long-term problems of discs compressed by the tether and the possibility of late-onset back pain.
Disclosure: Dr Hsu co-owns a patent and is co-developer of a vertebral body tethering system