Big e-referral contracts are shifting from old tech to more flexible, secure and efficient solutions. What follows?
There was big news this week in the winning of a major e-referral outpatient contract for the Alfred group of hospitals and community centres in Melbourne by cloud-based e-referral and guidance advice solution, Consultmed.
What does that mean for GPs? Potentially plenty, so bear with me.
Most e-referral solutions deployed around the country are using secure messaging delivery (SMD) platforms, some of which have proven to be controversial because the technology is old, has asynchronous point-to-point capability only, and delivers PDFs only at one end, making them inflexible.
Because of complex requirements for specific integrations to existing community healthcare provider platforms such as Best Practice, Medical Director and Genie, such deployments often have the effect of locking in a select few patient management system vendors and then nearly always only for only GPs and specialists.
This can stifle innovation, especially around the delivery of more flexible cloud-based solutions to interoperability in the system.
The Consultmed platform has integrations to all these older server-bound iterations of the major GP and specialist patient management systems, but it also has built for the future by creating the ability for these and other provider-based platforms to connect via Smart-on-FHIR technology.
In other words, the Consultmed solution is true SaaS, cloud-hosted, FHIR-enabled software, not a point-to-point SMD solution, which makes it a lot more flexible and a lot more future proof for hospitals thinking about how to rapidly evolve their e-referral connectivity, and their ability to talk more regularly and efficiently with the external specialist and GP community.
Significantly, Consultmed, which is a relatively small local scale-up, beat out the likes of incumbent e-referral sector heavyweights HealthLink, Salesforce, Novari Health, and Global Health, and a few large consulting firms that have proposed Microsoft Dynamics solutions.
What appears to have gotten Consultmed over the line are a few distinct advantages their cloud-first platform is bringing to the e-referral game: secure and easy bi-directional communication capability, “advice and guidance” functionality (above and beyond the straight Smartform e-referral ability) and a cloud-based portal that makes the functionality available far wider into community healthcare providers than just the GP and specialist community.
The Alfred tender called for “advice and guidance” functionality over and above the basic e-referral capability.
“Advice and guidance” (A&G) is a concept that is well established in some overseas countries – in particular the UK now – and which is garnering significant interest now in Australia in various hospital management jurisdictions for its potential to significantly improve the efficiency of outpatient services.
It is essentially technology which allows far more meaningful and efficient non-face-to-face communications between a hospital and the local GPs, specialists and other allied health professions servicing the hospital via secure synchronous and asynchronous cloud-based communication protocols.
By facilitating such additional communication capability in a manner that is efficient for both the hospital and the servicing specialist or GP, it allows providers to easily ask a GP, specialist or even a relevant allied health provider, for advice on a treatment plan, clarify a patient’s test results, check on the appropriateness of an outpatient referral and identify the most clinically appropriate service to refer a patient to within a region or a hospital.
It is currently thought that up to a third of current hospital outpatient referrals could be avoided by better initial communication between the community-based provider and the relevant hospital.
Related
In the UK, A&G platforms are now at the centre of a major push to significantly enhance the efficiency of outpatient services, mostly by improving the basis of shared decision-making between a hospital and its relevant local community-based healthcare providers.
The UK has a target in that system to reduce face-to-face outpatient services over the next five years by over 30%, which would amount to more than 30 million outpatients visits per year.
If you visit the Alfred website today, you can easily get an immediate sense of how transformative a cloud-based e-referral system and A&G platform might end up being to this hospital precinct within a short timeframe if deployed properly.
Below is what a patient currently has to go through to access the Alfred’s Diabetes Connected Care Clinic:
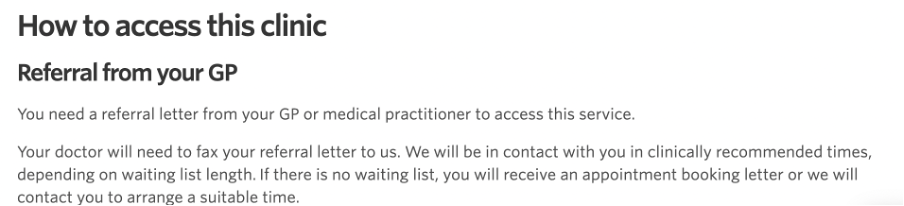
If the Consultmed platform works in the manner they say it does, you can imagine that understanding whether you actually need to use this clinic and accessing it will be a lot quicker and easier in the not-too-distant future.
The other big advantage of the Consultmed solution seems to be that, while it also has direct integrations to the major GP and specialist patient management systems, like SMD-based solutions do, being cloud-based any community-based provider can log into the Consultmed portal directly and use the system to talk to their local hospital network.
This means that the solution isn’t just available to local GPs and specialists but to any relevant allied health vendor that wants to use the system, a trend that is becoming increasingly prevalent as team-based chronic care management in the community takes hold.
Although small, Consultmed has now won enough e-referral type contracts across the country for analysts to start to wonder if finally the old and inflexible SMD paradigm for communicating between hospitals, GPs and specialists, might now be starting to truly break down, something that has been forecast by pundits for nearly a decade now but has so far not really eventuated.
The emergence of the more flexible cloud-based platform of Consultmed also synchronises reasonably well to plans from with the Department of Health and Aged Care and the Australian Digital Health Agency to drive all providers and local technology vendors to standardise within a short period of time to cloud-enabled web-sharing protocols such as FHIR and open APIs.
Consultmed has had a significant contract with the Sydney Children’s Hospital Network for two years already so is building a performance dataset they are able to showcase with other hospital groups for them to demonstrate just how well their platform works to increase efficiency and potentially reduce outpatient referrals.
It has also won the e-referral business for all five NSW PHNs who want to help prime the ability of GPs in their regions to easily refer their complex mental health patients, first to local PHN-backed Head to Health facilities, and then to other relevant parts of the local health networks. In this set of contracts all these PHNs are funding their local GP practices to integrate with Consultmed.
Now that they’ve won a big Victorian network, have an existing NSW hospital network and all five NSW PHNs, there will likely start to be pressure on the big centralised NSW e-referral project called the Engage Outpatient referral management platform which relies on old SMD technology to work.
Reportedly the development of this statewide e-referral platform has cost NSW Health something like $20 million, but already the LHD which piloted the platform has chosen not to go ahead with using it.
The project was controversial from the outset because it’s all based on the old SMD technology, via a major contract with one of the biggest national SMD providers in the country, Healthlink.
If Sydney Children’s Hospital Network has already broken ranks, if all NSW PHNs are using the Consultmed cloud-based alternative, and with the Alfred contract now in play it may not be long until other NSW LHDs start doing their homework and deciding that it may be much more effective and less expensive for them to skip the trouble of socialising an old SMD platform with their local GP and specialist communities for their e-referrals and move to a more efficient, more flexible cloud-based solution like Consultmed.
The same might be true of several Queensland hospital networks, some of whom are now trialling bespoke solutions using Salesforce technology and a major (and often expensive) consultant to help with integration.
Note: The topic of transitioning from old secure messaging and patient management system platforms to more flexible and efficient cloud-based platforms will be discussed in detail at the upcoming Wild Health Connected Care Summit in Melbourne on October 22.
You can view the whole program and get tickets HERE.
There aren’t many tickets left but if you are an HSD subscriber you automatically qualify for a 20% discount on any ticket type using this promo code HSD20.
If you have any issues getting your ticket or other questions on the summit contact greta@healthservicesdaily.com.au