The increase in risk existed regardless of age, gender and previous psychiatric illnesses.
A good doctor-patient relationship can be key to mitigating risks.
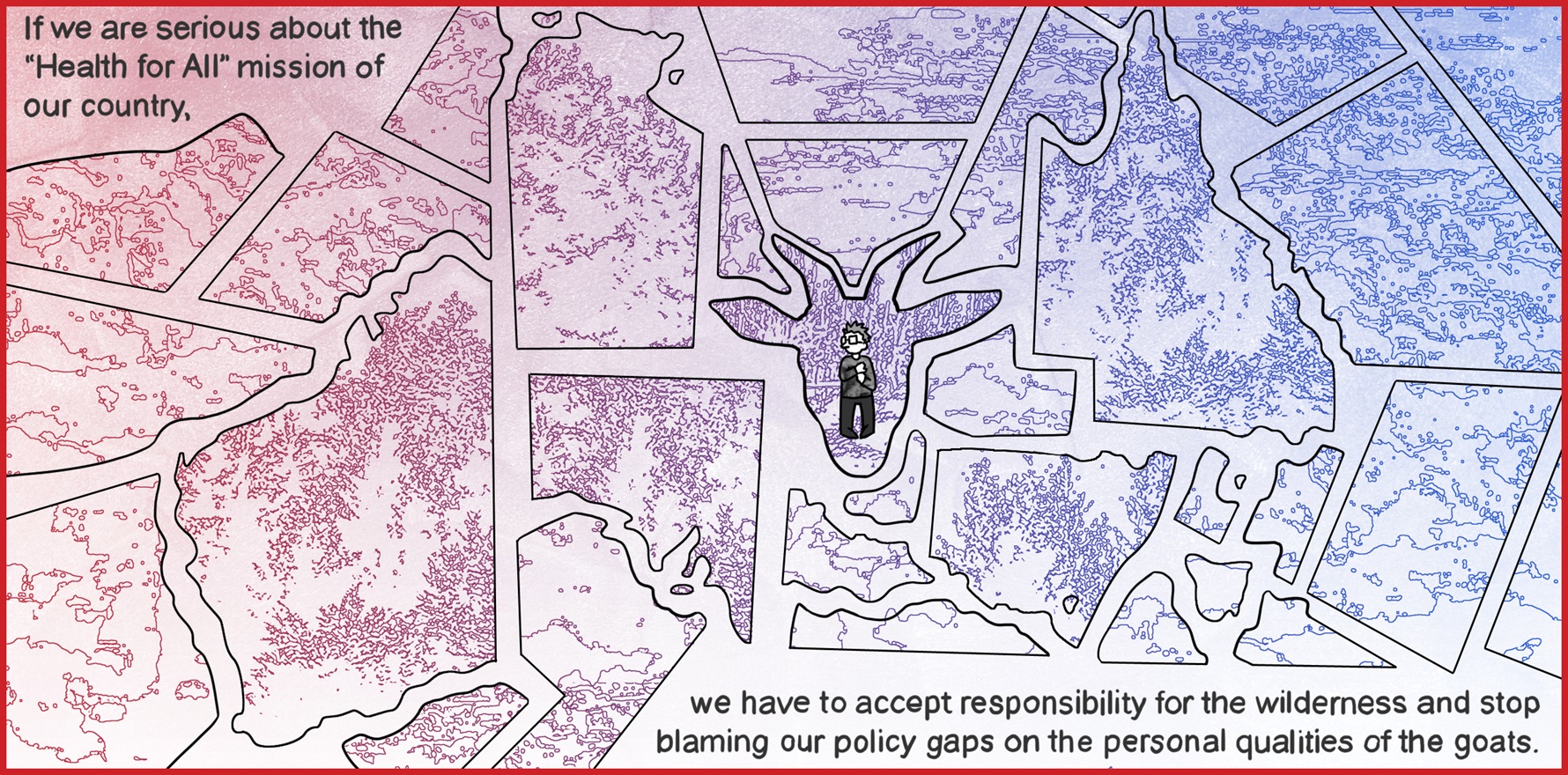
General practice is a critical part of suicide prevention, but scientific and anecdotal evidence linking the likelihood of GP consultations with suicide risk does not align.
Previous studies suggest those who suicide have greater engagement with their GP prior to their death; experienced GPs may say the opposite – where it’s the patients you don’t see that you should be concerned about.
A new UK case-control study found consulting a GP more than once per month over a 12-month period was associated with a 5.9-fold increase in the odds of committing suicide – irrespective of age, sex and a history of psychiatric conditions. The findings were published in the British Journal of General Practice.
“This study highlights the importance of a good doctor-patient relationship and longitudinal care, which leads to better health outcomes,” said Dr Cathy Andronis, chair of the RACGP’s specific interest psychological medicine group.
“It’s easier for patients who have a trusting relationship with their doctor to be more honest about how they’re feeling, but it also means the doctor is more able to notice when patients become distressed, or if they’ve stopped coming in as often as they used to.”
Researchers identified 14,000 patients who died by suicide and compared their primary care consulting patterns in the year before their death with up to 40 live controls (per patient) who were registered at the same practice, for a total of nearly 600,000 patients.
After adjusting for age and sex, patients who consulted their GP 13 or more times in the year before their death had a 5.9-fold increase in the odds of suicide compared to patients who only had one consult. Patients who did not consult their GP in the 12 months leading up to suicide had a 35% decrease in the odds of suicide.
“We speculate that frequent consultations could indicate increases in disease severity, unresolved medical complaints or ongoing psychosocial stressors manifesting as psychological or physical complaints,” the researchers concluded.
Age, sex, socioeconomic status and a history of psychiatric illness all modified the association between the number of consultations and suicide.
Having 13 or more consults in the year prior to death increased the odds of suicide 5.3-fold for males compared to male patients who only had one visit in the year prior to their death but increased the odds 9.5-fold compared to females who only saw their GP once in the year before their death. Similarly, having 13 or more consultations increased the odds of suicide 8.1-fold in patients aged 15 to 44 compared to patients who had one consultation over a 12-month period, but only 2.9-fold for patients over the age of 75.
Researchers felt the increased suicide risk was related to females and younger individuals being more likely to present to their GP despite generally having a lower risk of suicide, but Dr Andronis said the findings didn’t provide a lot of new information about suicide risks for our most vulnerable population.
Related
“We already know younger people and women come [to their GP] more often, but 75% of suicides in Australia are male, so we’re still failing to pick up the biggest at-risk group,” she told TMR.
Eighty-six percent of the patients who suicided had at least one consultation in the 12 months before they died, compared to 77% of controls.
The five most common reasons for consultation in the year before suicide were medication review and requests (11.9%), depression, (7.3%), pain complaints (6.3%), mental health assessment and care (4.1%), and overdose (3.1%). Self-inflicted injuries were the seventh most common reason for consultation (2.7%).