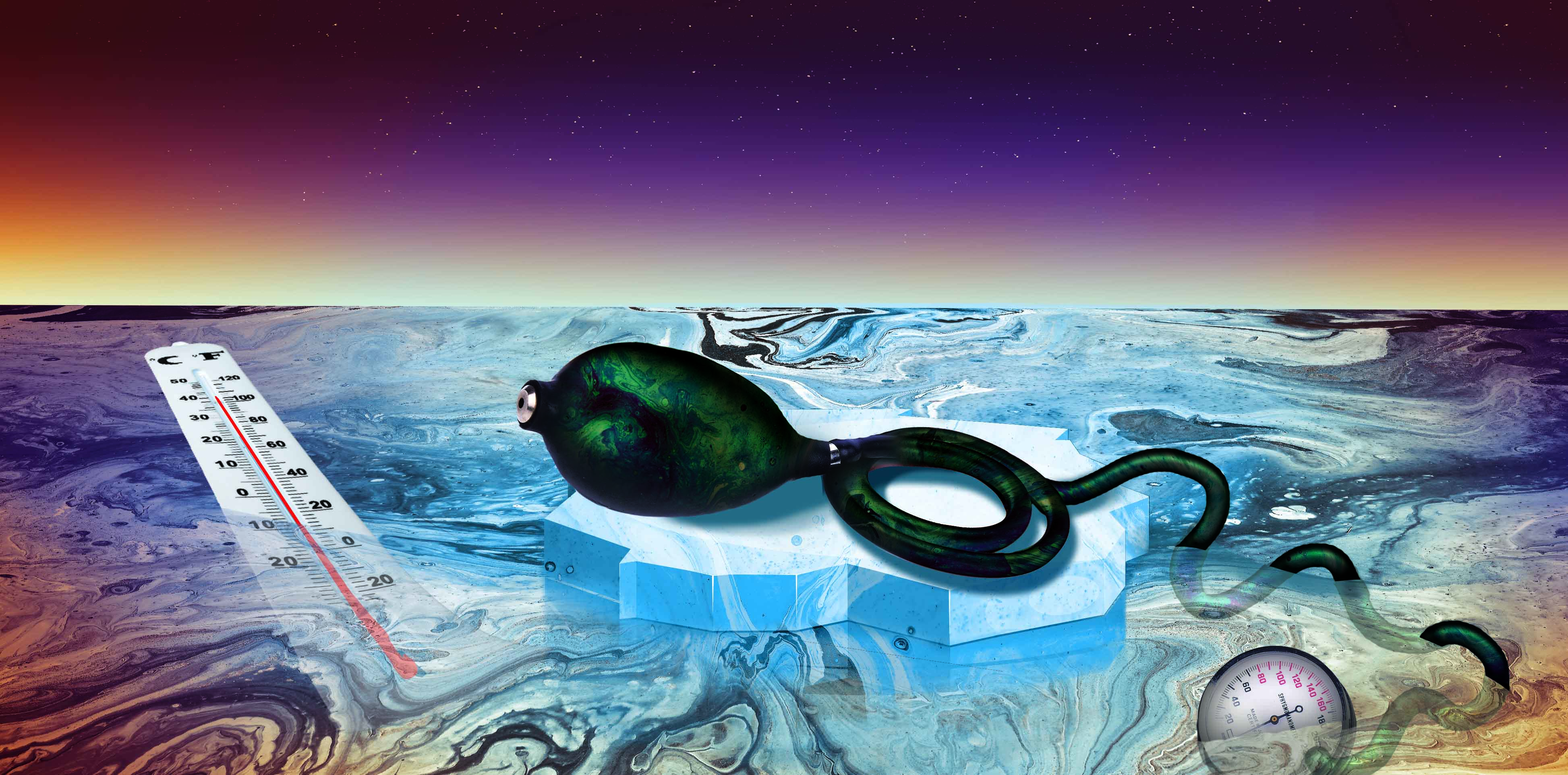
With the reality of climate change taking hold, what are the implications for the management of hypertension?
Australians are facing more extreme and more variable temperatures than at any point in human history as a result of anthropogenic climate change. According to the Australian Bureau of Meteorology, Australia has recorded eight of its hottest years in the last decade. It also warns that the number of heatwaves since December 2018 has been unusually high.
Such rapidly changing temperatures could have more wide-reaching health impacts than first thought. Researchers are starting to see that heat fluctuations can have dramatic effects on cardiovascular health, as well as on other conditions, and it is critical that medical researchers and clinicians start to prepare for these unprecedented environmental perturbations.
So what exactly does mean for the health of Australians, particularly those with chronic illnesses?
It could have a profound impact on the epidemiology of hypertension and cardiovascular disease, emerging research suggests.
One reason for this is that a hotter and more variable climate may significantly affect seasonable blood pressure (BP) variability and increase the risks of cardiovascular disease, especially in those with high cardiovascular risk and the elderly.
We know from our own analysis of over 500 of the 4600 participants from the AusDiab conducted in 2012 (1) that hypertension is under-diagnosed and poorly controlled.
Using the gold standard method of ambulatory BP, we found that as many as 43% of the group were classified as hypertensive, yet only 25% were taking antihypertensive therapy.
Among those who were treated, 9% still had hypertension, and this was three times more common in men than in women. This means that a staggering 36% of that study cohort had not reached target levels of BP. (1)
Since 2012, our country has experienced the hottest period on record.
This is troubling, because a study on the impact of extremely hot days on emergency department visits by older adults in New York State between 2005 to 2013 found that there was a7% increased risk of ischaemic heart disease and a 4% greater risk of hypertension w (2) For New York in summer, this was only 28oC.
Interestingly, the peak of cardiac dysrhythmias occurred six days after the event, (2), indicating there is a need for clinical vigilance not only on extremely hot days, but also for a considerable period after the event.
Closer to home, a study of 1.5 million emergency department admissions from five regions of NSW found that on the 99th percentile temperature days, not only was dehydration two-fold more likely to be reported within a few days of the extreme heat, but cardiovascular disease was also 14% more likely reported as an underlying condition. (3)
We have known for a very long time that seasonal variations in BP are real (4) and have implications for patients who have, or are at risk of, hypertension, stroke and cardiovascular disease in general. (5)
A recent review and consensus statement from the European Society of Hypertension Working Group on BP Monitoring and Cardiovascular Variability analysed the evidence for the seasonal variation in BP and included the magnitude, epidemiology, pathophysiology, and importantly the relevance of the changes. (6) They concluded that BP is usually several mmHg lower during the summer and higher during the cold season.
Office measurements of systolic BP/diastolic BP is 5.3/3.3mmHg on average in the summer compared with the winter.
The effect is global and affects all age groups, sexes and ranges of BP, from normotensive levels to each of the categories of hypertension. Interestingly, night-time BP is slightly higher in summer than winter by 1.3/0.5mmHg, which is the opposite to its effect on daytime BP. This means that the day-to-night difference in BP, which is known as the nocturnal “dipping” status of a patient, is decreased in summer and increased in winter. (6)
In addition, the morning surge of BP is known to be greater in winter due to the nocturnal BP decline. (7) Morning BP surge is well known to be an independent predictor of cardiovascular events, including stroke. (8, 9) Interestingly we found a particular risk in Japanese women with those in the higher BP surge quintile being nearly three-fold more likely to experience a non-fatal stroke and two-fold more likely to have a cardiovascular event. (9)
The seasonal difference in BP between the colder and warmer months may increase the incidence of hypertension and reduce the hypertension control rate in winter. This would presumably increase cardiovascular risk, particularly in those with chronic cardiovascular disease.
So, what can be done to improve the health of these patients?
The recommendation for hypertensive patients from European Society of Hypertension consensus group is that if symptoms consistent with over-treatment appear with temperature rise or a BP rise is observed during cold weather, some modification to the treatment regime may be warranted.
They recommend that BP changes should be confirmed with out-of-office techniques, preferably ambulatory BP or home monitoring. (6) Importantly, other possible causes of the change should also be investigated and excluded. If symptomatic hypotension is evident, down titration of treatment should be considered. However, the group also noted that further research is needed for the best management of the influence of seasonal BP changes.
Sungha Park, from Yonsei University in Korea, and colleagues from the HOPE Asia Network, recently reviewed the influence of ambient temperature on hypertension in Asia and cautioned against down titration or reduction in the number of medications in summer since nocturnal BP was not reduced. (10) In clinical practice, antihypertensive agents tend to be reduced in summer to avoid excessive decrease in BP.
Diuretics are commonly reduced in elderly hypertensive patients with underlying chronic kidney disease, who are deemed to be at high risk of dehydration and acute kidney injury in summer, (11) and those with diabetes who are deemed a high risk of orthostatic hypotension. (12) For medical practitioners, plasma sodium and urea are reliable markers of these conditions and useful when deciding the down titration.
For patients, it is recommended to measure not only home BP, but also the daily weight to monitor the fluid status to detect early dehydration.
The most important point is to consider the possible implications of not only normal seasonal effects on patients, but also extreme weather events. We suggest that clinicians exercise vigilant care for patients with hypertension, particularly those that are elderly and those with relevant co-morbidities such as kidney disease.
We also recommend more frequent measurement of BP, particularly using out-of-office assessments in order to minimise the white-coat effect and to diagnose masked hypertension.
But it’s not only hypertension that we should be worried about.
A study from the School of Public Health, Faculty of Medicine, University of Queensland, published in 2020, examined the effect of hourly differences in temperature on the risk of acute kidney injury. (13) Males and the elderly, particularly those with diabetes, hypertension, heart failure or chronic kidney disease, were two to three times more likely to be at risk of acute kidney injury after exposure to an acute heat event. (13)
A study from the University of California on the effect of ambient temperature and heatwaves on hospitalisations in California found that higher temperatures were associated with more admissions for acute renal failure, dehydration, ischaemic stroke and primary diabetes .
They also found that heatwaves independently predicted a . (14) However, the risks may be even higher, as this nearly decade-old study used a definition of heatwaves that we might now consider not so extreme.
Cardiologists in the Indian province of Tamil Nadu very recently reported a very high (24%) prevalence of atrial arrhythmias in patients who had suffered heat stress (15). In this province during April and May, the average temperature is above 39oC with maximums of 45oC.
As the climate transitions and extremes of temperature become increasingly more frequent, we clearly need to have a better understanding of the risks for cardiovascular health particularly for the elderly and also those with underlying disease such as diabetes or renal disease.
There are many questions we still don’t have a clear answer on, such as whether long term outcomes will be improved if we adjust antihypertensive pharmacotherapy according to season or even in the shorter-term during heat waves.
There are also other conditions, such as dehydration and its associated impact of renal function, as well as cardiac arrhythmias, that need to be considered.
Clearly, we need to be able to provide evidence-based, clear and consistent messages to the medical practitioners based on quality research on the likely impact of climate and weather events on their patient’s condition.
The European Society of hypertension has provided an up-to-date consensus statement of seasonal variation and BP, but we also need to widen this to consider our changing climate.
Professor Geoffrey A. Head is Chair of the Australian Ambulatory Blood Pressure Collaborative Head, Neuropharmacology Laboratory, Baker Heart and Diabetes Institute and NHMRC Principal Research Fellow, Adjunct Professor, Monash University
Dr Yusuke Sata is Senior Research Fellow, Baker Heart and Diabetes Institute Cardiologist, Alfred Hospital, Melbourne, and Senior Lecturer, Faculty of Medicine, Nursing & Health Sciences, Monash University
References:
- Head G, Shaw J, Dunstan D, Owen N, Magliano D, Chadban S, et al. Hypertension, white-coat hypertension and masked hypertension in Australia: findings from the Australian Diabetes, Obesity, and Lifestyle Study 3. J Hypertens 2019;37(8):1615-1623.
- Li M, Shaw BA, Zhang W, Vasquez E, Lin S. Impact of Extremely Hot Days on Emergency Department Visits for Cardiovascular Disease among Older Adults in New York State. Int J Environ Res Public Health 2019;16(12).
- Khalaj B, Lloyd G, Sheppeard V, Dear K. The health impacts of heat waves in five regions of New South Wales, Australia: a case-only analysis. Int Arch Occup Environ Health 2010;83(7):833-42.
- Rose G. Seasonal variation in blood pressure in man. Nature 1961;189:235.
- Modesti PA. Season, temperature and blood pressure: a complex interaction. Eur J Intern Med 2013;24(7):604-7.
- Stergiou G, Palatini P, Modesti P, Asayama K, Asmar R, Bilo G, et al. Seasonal Variation in Blood Pressure: Evidence, Consensus and Recommendations for Clinical Practice, Consensus Statement by the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J Hypertens 2019:doi: 10.1097/HJH.0000000000002341 Epub ahead of print.
- Murakami S, Otsuka K, Kono T, Soyama A, Umeda T, Yamamoto N, et al. Impact of outdoor temperature on prewaking morning surge and nocturnal decline in blood pressure in a Japanese population. Hypertens Res 2011;34(1):70-3.
- Luo Y, Wang Y-L, WU Y-B, Liang Y-L, Head GA, McGrath B, et al. Association between the rate of the morning surge in blood pressure and cardiovascular events and stroke. Chin Med J 2013;126(3):510-4.
- Head G, Sata Y, Imai Y, Kikuya M, Ohkubo T, Reid C, et al. Moderate morning rise in blood pressure has lowest risk of stroke but only in women. J Hypertens 2019;37(7):1437-1447.
- Park S, Kario K, Chia YC, Turana Y, Chen CH, Buranakitjaroen P, et al. The influence of the ambient temperature on blood pressure and how it will affect the epidemiology of hypertension in Asia. J Clin Hypertens (Greenwich) 2019.
- Imai E, Abe K. Blood pressure drop in summer may cause acute kidney injury with irreversible reduction of glomerular filtration rate. Clin Exp Nephrol 2013;17(1):1-2.
- Sega R, Cesana G, Bombelli M, Grassi G, Stella ML, Zanchetti A, et al. Seasonal variations in home and ambulatory blood pressure in the PAMELA population. Pressione Arteriose Monitorate E Loro Associazioni. J Hypertens 1998;16(11):1585-1592.
- Xu Z, Hu X, Tong S, Cheng J. Heat and risk of acute kidney injury: An hourly-level case-crossover study in queensland, Australia. Environ Res 2020;182:109058.
- Sherbakov T, Malig B, Guirguis K, Gershunov A, Basu R. Ambient temperature and added heat wave effects on hospitalizations in California from 1999 to 2009. Environ Res 2018;160:83-90.
- Paul A, Alex R, Jacob JR, Yadav B. Effects of heat stroke on surface ECG: a study on clinical outcomes. Heart Asia 2019;11(2):e011221.