Insights from the 2022 National Roundtable Report and practical tools for cholesterol management.
Evidence landscape, identified barriers from a recent National Roundtable on Cholesterol, and practical resources to better manage cholesterol along with other CVD risk factors in your patients.
With approximately 6.5 million adults living with the condition, high cholesterol accounts for a significant burden of heart disease and stroke in Australia.1,2 This is despite clear evidence that an individual’s risk of atherosclerotic cardiovascular disease (CVD), including stroke, increases as low-density lipoprotein cholesterol (LDL-C) increases.3,4
High cholesterol is responsible for more than one third of all the years of healthy life lost by Australians due to heart disease.5 Yet, almost half of Australians presenting to general practice with CVD (mainly coronary heart disease or stroke) are not achieving recommended cholesterol levels, even though most are prescribed lipid-lowering medicines.6 Younger adults, women, and individuals prescribed fewer than four evidence-based therapies or not prescribed intensive lipid-lowering therapy are less likely to reach ideal lipid targets. 6,13
Australian guidelines currently recommend an LDL-C target of <2 mmol/L for primary prevention and <1.8 mmol/L for secondary prevention.7 More recently, some international guidelines recommend a more intensive LDL-C target of <1.4 mmol/L in the secondary prevention setting. 8
Healthy lifestyle changes including diet, physical activity, smoking cessation and weight management are recommended as first-line management strategies for all individuals. Where lipid-lowering medicines are indicated, statins remain the first-line agents of choice within the context of cardiovascular risk reduction.9
Despite the proven efficacy of lipid-lowering medicines and lifestyle measures, many Australians are not receiving interventions to achieve target cholesterol levels to prevent heart disease and strokes.6,10-13 To address this, the Heart Foundation held a national roundtable on cholesterol in June 2022, in partnership with the World Heart Federation, which provided insight into the roadblocks to cholesterol management in Australia.
The following barriers were identified at the clinician level:14
- Competing priorities in general practice (time pressure, patients with multiple conditions, GP shortages)
- Lack of confidence when escalating lipid-lowering medicines
- Gaps in knowledge and education on cholesterol management
At the consumer level, several barriers were also identified, including medicine non-adherence. Non-adherence is as high as 67% at 12 months after initiation of treatment,15 which is significant given that non-adherence to CVD medicines is associated with increased mortality.16 Non-adherence to statin therapy in particular is associated with a three-fold increase in mortality after an acute coronary syndrome diagnosis.11
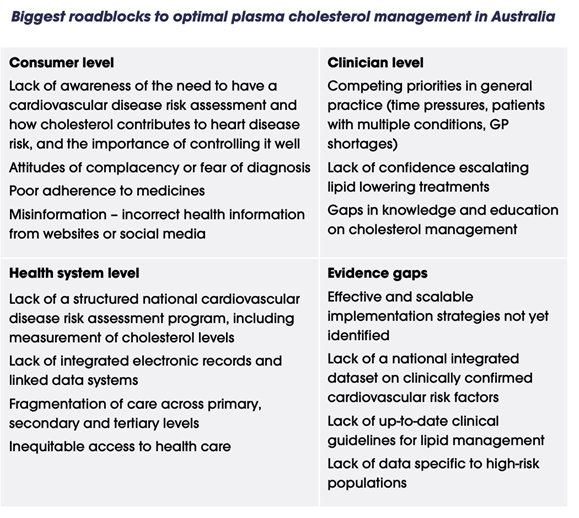
Adapted from ‘Cholesterol roadblocks and solutions: Report from Australia’s National Roundtable on Cholesterol’, 202214
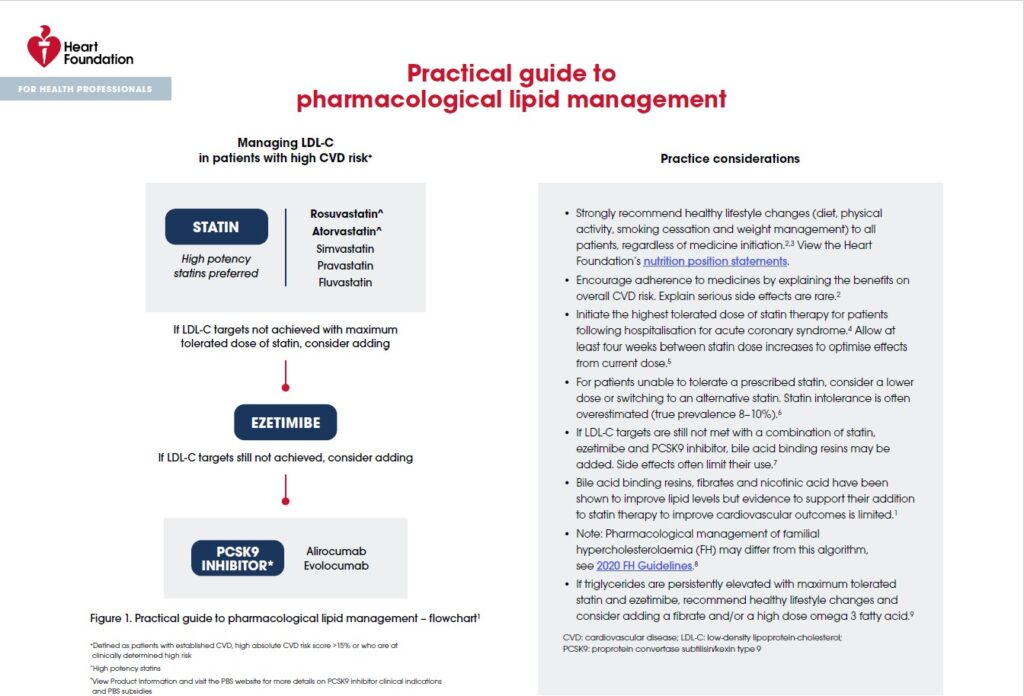
To support GPs in managing patients with high cholesterol, the Heart Foundation offers an easy-to-use practical guide to pharmacological lipid management, which provides:
- a flowchart with recommendations on prescribing lipid-lowering medicines (statins, ezetimibe and PCSK9 inhibitors) and when to escalate treatment
- key considerations when prescribing lipid-lowering medicines
- a comparison of the lipid-lowering potential of individual medicines.
Download here
This guide comes as part of the Heart Health Check Toolkit, which has been used by over 100,000 health professionals across Australia to routinely assess and manage CVD risk with ease. With ready-to-use templates embedded in practice software like Bp Premier and MGT app, the Heart Health Check Toolkit makes it easier to manage key risk factors such as high cholesterol, and is integrated with healthy living resources for your patients.
A new Australian guideline for the assessment and management of CVD risk is also currently in development and will be available mid-2023.
By routinely conducting Heart Health Checks and supporting your patients to make healthy lifestyle changes, general practice teams are making measurable, life-saving impact in the fight against CVD in Australia. Make good use of the Heart Health Check Toolkit today to streamline your pivotal work in CVD prevention.
Want to know the Toolkit better? A four-part email journey is available now to familiarise you with the Toolkit’s many templates and resources. Sign up here to receive practical tips that will help you integrate the Toolkit into routine preventative care.
References
- Australian Bureau of Statistics. Australian Health Survey: Biomedical Results for Chronic Diseases. 5 August 2013. Available from: abs.gov.au/statistics/health/health-conditions-and-risks/australian-health-survey-biomedical-results-chronic-diseases/2011-12#cardiovascular-disease
- Australian Bureau of Statistics. Population by age and sex – national. Summary statistics of Australia’s population by age and sex. 26 Sept 2022. Available from: abs.gov.au/statistics/people/population/national-state-and-territory-population/mar-2022
- A Murphy, JP Faria-Neto, K Al-Rasadi et al., ‘World Heart Federation cholesterol roadmap’, Glob Heart, 2017, 12(3):179–197
- F Mach, C Baigent, AL Catapano, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 2020; 41(1):111-188. doi:10.1093/eurheartj/ehz455
- Australian Institute of Health and Welfare. Australia’s health. Snapshot: Biomedical risk factors. 7 July 2022. Canberra: AIHW; 2022. Available from: aihw.gov.au/reports/australias-health/biomedical-risk-factors
- N Alsadat, K Hyun, F Boroumand, et al. Achieving lipid targets within 12 months of an acute coronary syndrome: an observational analysis. Med J Aust 2022; 216(9):463-468. doi:10.5694/mja2.51442
- National Vascular Disease Prevention Alliance. Guidelines for the management of absolute cardiovascular disease risk. 2012. heartfoundation.org.au/conditions/fp-absolute-cvd-risk-clinical-guidelines
- National Heart Foundation of Australia & Cardiac Society of Australia and New Zealand. Australian clinical guidelines for the management of acute coronary syndromes 2016. Heart Lung Circ. 2016;25(9):895-951. doi:10.1016/j. hlc.2016.06.789
- Therapeutic Guidelines Limited. Therapeutic Guidelines: Cardiovascular 2018. eTG. March 2021 ed: Therapeutic Guidelines Limited; 2021
- F Mach, C Baigent, AL Catapano et al., ‘2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk’, Eur Heart J, 2020; 41(1):111–188.
- J Allonen, MS Nieminen, M Lokki, O Parkkonen, S Vaara, M Perola, T Hiekkalinna, TE Strandberg, J Sinisalo. Mortality rate increases steeply with nonadherence to statin therapy in patients with acute coronary syndrome. Clin Cardiol. 2012;35(11):E22–E27. doi: 10.1002/clc.22056
- CM Hespe, A Campain, R Webster et al., ‘Implementing cardiovascular disease preventive care guidelines in general practice: an opportunity missed’, Med J Aust, 2020, 213(7):327–328
- D Brieger, M D’Souza, K Hyun et al., ‘Intensive lipid-lowering therapy in the 12 months after an acute coronary syndrome in Australia: an observational analysis’, Med J Aust, 2019, 210(2):80–85
- Heart Foundation, ‘Cholesterol roadblocks and solutions: Report from Australia’s National Roundtable on Cholesterol’, Heart Foundation website, 2022, accessed 28 October 2022. www.heartfoundation.org.au
- LA Simons, ‘An updated review of lipid-modifying therapy’, Med J Aust, 2019, 211(2):87–92
- JN Rasmussen, Chong A, Alter DA. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. J Am Med Assoc. 2007;297(2):177–186. doi: 10.1001/jama.297.2.177