Australian hysterectomy rates – the most radical solution – have dropped 20% since 2014, but remain far higher than in the UK and NZ.
A revised clinical care standard for heavy menstrual bleeding now explicitly recommends initiating medication for symptom relief at first presentation, even as investigations are ongoing.
The care standard was released today by the Australian Commission on Safety and Quality in Healthcare, alongside a report looking at women’s health across the country.
According to GP Associate Professor Liz Marles, a clinical director at the Commission, the changes from the original 2017 standard are relatively minor.
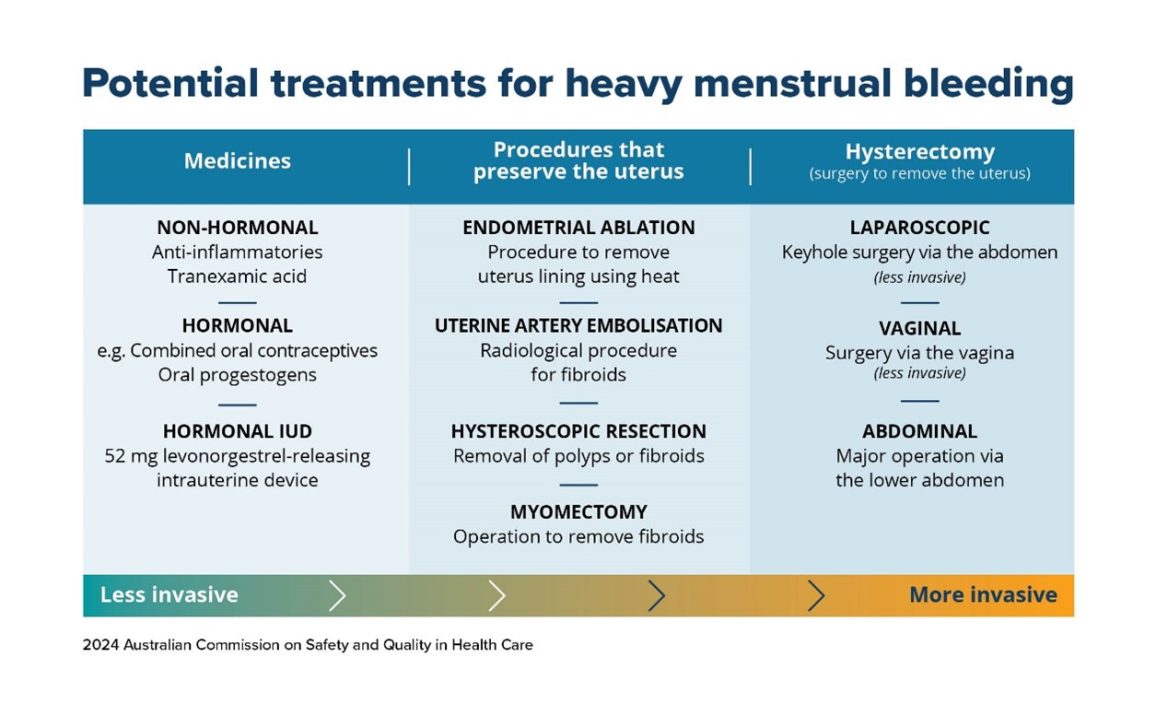
“We’ve got a particular focus on assisting women to make an informed choice, and the treatment options section has been expanded … [with] a little bit more about uterine artery embolisation as a treatment option,” she told The Medical Republic.
“We have introduced a new section on cultural safety and equity, which I think is really important in light of the higher rates of hysterectomy among First Nations women.”
The revision that will make the most immediate change on a practical level, she said, is the clearer guidance on commencement of oral therapies for symptom management.
“You can start treatment [with tranexamic acid or anti-inflammatories] as soon as a woman raises her heavy menstrual bleeding, whilst you continue to do investigations as to what the underlying cause may be,” Professor Marles said.
“We don’t need to put off giving them something simple like that just because we’re yet to do an ultrasound.
“For instance, we can get started on the tranexamic acid and go ahead and organise the ultrasound for some time in the future.”
Related
Research done in conjunction with the updated clinical standard found that around two-thirds of women with heavy periods did not seek medical care and that they were generally unaware of the range of treatment options outside of hysterectomy.
That’s not to say there isn’t positive change; there’s been a 10% rise in the rate of women getting the less invasive endometrial ablation treatment since 2014.
Hysterectomy rates across Australia have also dropped by 20% over the same period, from 290 per 100,000 women to 231.
For comparison, the hysterectomy rate per 100,000 women in the UK is 132, while the New Zealand rate is 126.
“Hysterectomy is absolutely the most invasive and permanent solution to [heavy bleeding] and is also probably the most costly treatment with the most risks associated with it,” Professor Marles said.
“The opportunity to offer less invasive options and to treat this at an earlier stage is something that we’re trying to promote.”
Rural and regional Australians had consistently higher rates of hysterectomy, and the rate among First Nations women is almost 10% higher than baseline.
It’s unclear exactly why this may be.
“There’s a five-fold difference in hysterectomy rates across the country, and this suggests that women are being treated differently,” gynaecologist and obstetrician Professor Kirsten Black told TMR.
“There are a number of potential factors, like access to services, counselling about options and [maldistribution of] practitioners skilled in less invasive techniques.”
Professor Black, who was also involved in the research backing the clinical care standard, said one of the key takeaways for her was the relatively low proportion of women who did not seek treatment for their heavy periods.
“There are still quite a lot of women who … just assume it’s normal,” she said.
Taking a detailed history is one way to combat this.
“It may be impacting their quality of life or resulting in low iron and anaemia, so we do need to … take a good menstrual history.”
Both Professor Marles and Professor Black said that while there was a lack of hard data, researchers hoped that the 2017 guidelines had contributed to the 20% drop in overall hysterectomies.