GPs should test for H. pylori before prescribing low-dose aspirin in patients at high risk of upper gastrointestinal bleeding, researchers say
Melbourne researchers have recommended that GPs test for Helicobacter pylori before prescribing low-dose aspirin in patients at high risk of upper gastrointestinal bleeding.
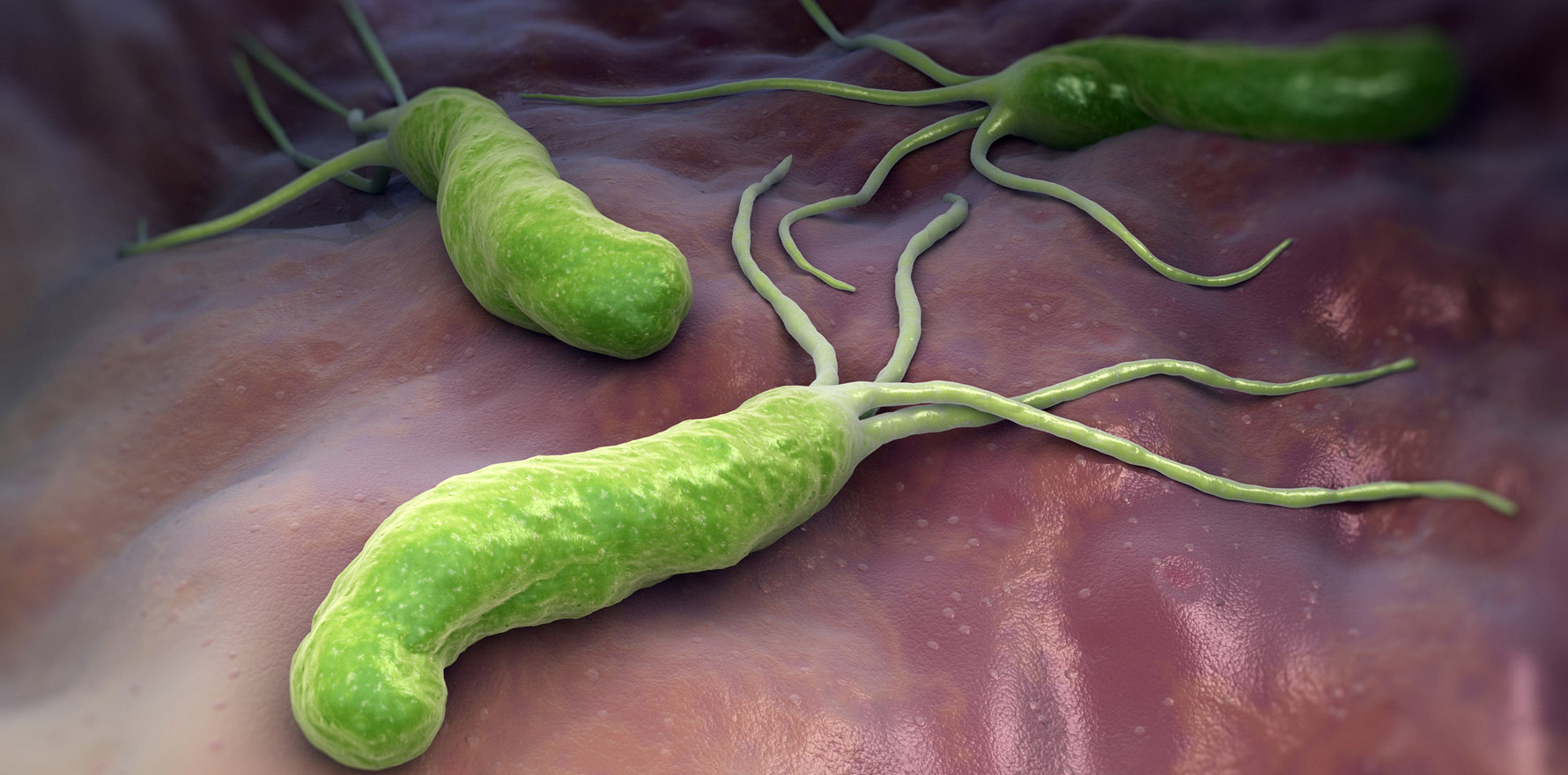
H. pylori infection doubled the odds of upper gastrointestinal bleeding in patients on low-dose aspirin, according to the first systematic review on the subject, published this month in the MJA.
H. pylori is the world’s most widespread infection, affecting around 40% of Australians aged over 60, and is known to be associated with peptic ulcers and haemorrhage.
Long-term use of anti-platelet medications such as aspirin also raises the risk of bleeding, so American and European guidelines recommend that patients be tested and treated for H. pylori prior to starting low-dose aspirin.
However, there has been only low-grade evidence to back up this recommendation until now.
“Our study, we are hoping, will add more weight to that recommendation,” lead author Dr Justin Ng, a medical resident at Peninsula Health in Melbourne, said.
Many Australian patients were taking low-dose aspirin for secondary or primary prevention of CVD – and a substantial proportion of these patients could have a concurrent, asymptomatic H. pylori infection, Dr Ng said.
If these patients were unfortunate enough to present to hospital with an upper GI haemorrhage, the mortality rate was quite high, despite advances in endoscopic and surgical techniques for controlling bleeding, he said.
However, the absolute risk of upper GI bleeding from low-dose aspirin was very low (less than 3.64 cases per 1000 person-years).
So, it probably was not a good allocation of resources to test every patient on low-dose aspirin for H. pylori, Dr Ng said.
The study estimated that GPs would have to test and treat between 100 and 1000 patients for H. pylori to prevent one bleeding event.
“We’re certainly not saying that every patient should be tested,” Dr Ng said. “But patients who have increased risk factors for having an upper gastrointestinal bleed … could benefit from having H. pylori tested and treated if positive.”
Patient who were at higher risk of bleeding included older patients, current smokers, patients on non-aspirin NSAIDs, those with a history of peptic ulceration or GI haemorrhage in the past.
H. pylori can be tested non-invasively through serology, a urea breath test, and a stool antigen test, or invasively through a biopsy.
Current therapeutic guidelines in Australia recommend the use of a PPI in combination with amoxicillin and clarithromycin (PPI-based triple therapy) as the first-line measure for eradication of H. pylori.