The following nine start-ups have a shared origin story: each was founded by people working on the frontlines of medicine
The following nine start-ups have a shared origin story: each was founded by people working on the frontlines of medicine. “They were seeing patients, they were identifying challenges and problems and they decided they could find solutions,” Dr Amandeep Hansra, GP and founder of Evermed consulting, said at the recent Wild Health Summit.
“And these solutions involved technology mostly, so telehealth, VR, blockchain, predictive analytics, AI – you name it.”
Each of these start-ups were given five minutes each to pitch their product at Wild Health. Here are the best takes:
Dr Rob Pearlman – Founder, MedApps
As a junior doctor moving from hospital to hospital, Dr Pearlman encountered a problem. Every hospital had different policies and procedures, and he couldn’t adapt fast enough.
“Five years ago, when I started my internship, I made a mistake,” he said.
He forgot to file some paperwork when requesting a CT scan, delaying the scan by a day and costing NSW Health $1,400. He was probably given instructions on what paperwork was needed in order a CT scan. “Possibly it was in my 120-page orientation manual,” he said. “But it goes to show that the convoluted nature of all that information.”
It’s hard to absorb all the administrative details quickly. This is no small issue: junior doctors move hospitals up to five times a year and there are 7,000 junior doctors across Australia. Dr Pearlman devised a solution in the form of a “modern hospital handbook”, a digital platform called Resident Guide that provides orientation information through a mobile app. Resident Guide is being deployed at 22 public hospitals across NSW and QLD, with over 2,500 users already. “We’re looking forward to taking Australia by storm,” Dr Pearlman said.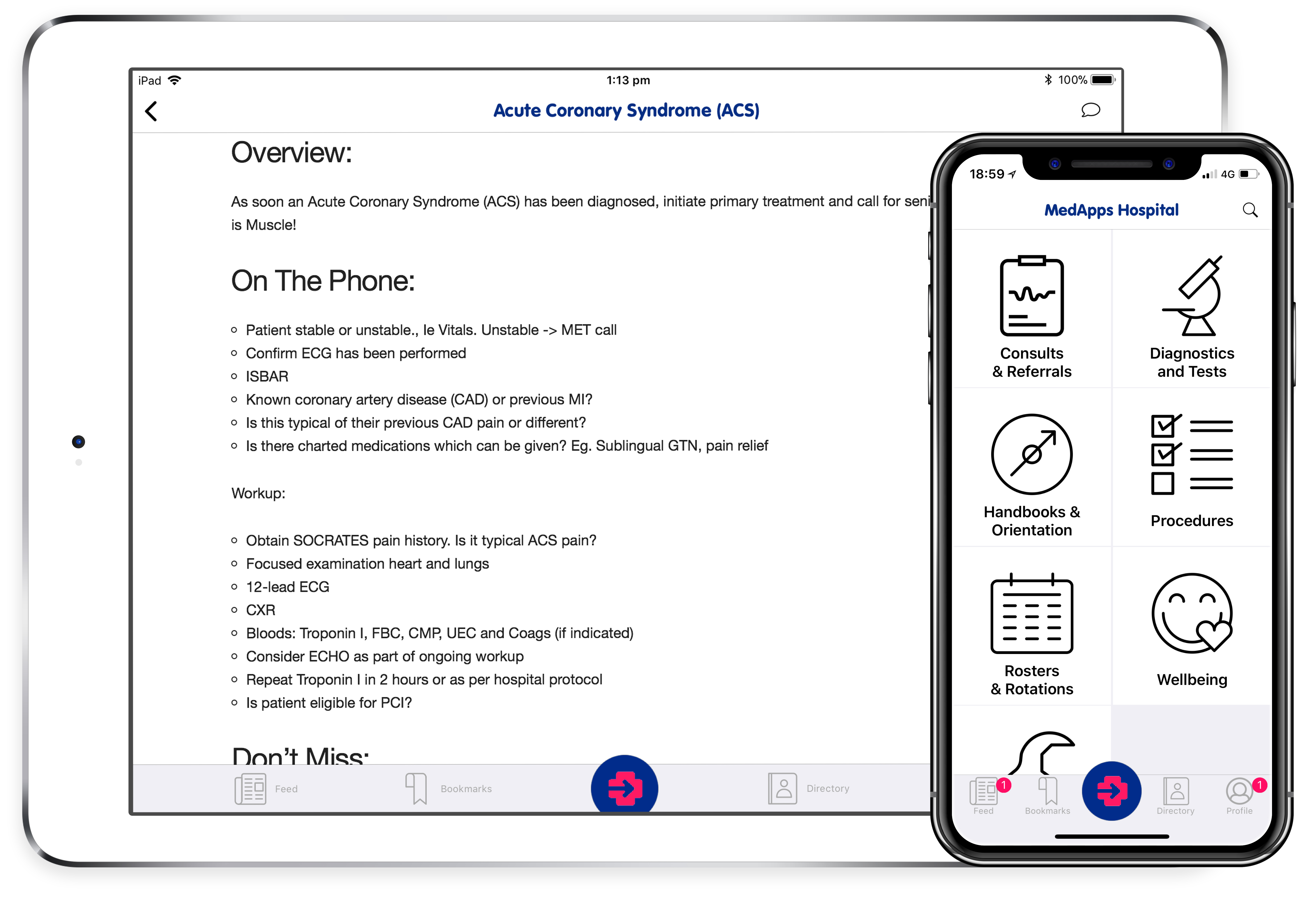

Dr Jonathan King – Founder & CEO, Lysn Health
Usually, patients have to wait several months to see a psychologist in person in Australia. Lsyn is a two-year old company that is helping patients find a psychologist within 24 hours. Patients can choose how to connect with their psychologists, either face-to-face, over the phone, over video link or by chatting online.
“We’ve now grown to 250 psychologists in the last year providing services nationally to 53 GP clinics,” said Dr Jonathan King. “It’s not just finding a psychologist in your postal code. What makes Lsyn different to all the other platforms that are helping you find someone who suits your needs.”

Dr Katja Beitat – CEO & Founder, Clinivid
A patient with a suspected brain bleed is transferred from a radiology practice to the emergency department. James, the ED doctor, uses Clinivid to request visual CT results from the radiologist. James can securely view the results on his phone or iPad and contact the radiologist to ask questions. Sounds easier than the current system of playing phone tag with specialists, doesn’t it?
Clinivid is offering a mobile-first, image and video-enabled service that allows clinicians to communicate to each other. Dr Beitat saw a link between delay or breakdown in communication and severe and serious consequences of patient care, and founded Clinivid as part of the solution. “The reality, we have incredible, beautiful systems out there but they don’t talk to each other,” she said.
“What we wanted to do was to link clinical systems that are already there with personal messaging in a way which is privacy-compliant, which is safe and which ticks all the boxes,” she said.

Elliot Smith – CEO & Co-Founder, Maxwell Plus
Maxwell Plus is a start-up based in Brisbane that is automating the detection of cancers by combining machine learning and medical imaging. Their first project is prostate cancer, which affects roughly one in every seven men in Australia. Using AI, the company is working to make prostate cancer diagnosis faster, more affordable and more accurate.
“We want to make sure that patients no longer have to worry about getting cancer because if it comes up, they know it’s going to be caught early, it’s going to be treated at the most appropriate time and they have a care team that they have a relationship with, managing that process and ensuring that they stay healthy,” Mr Smith said.

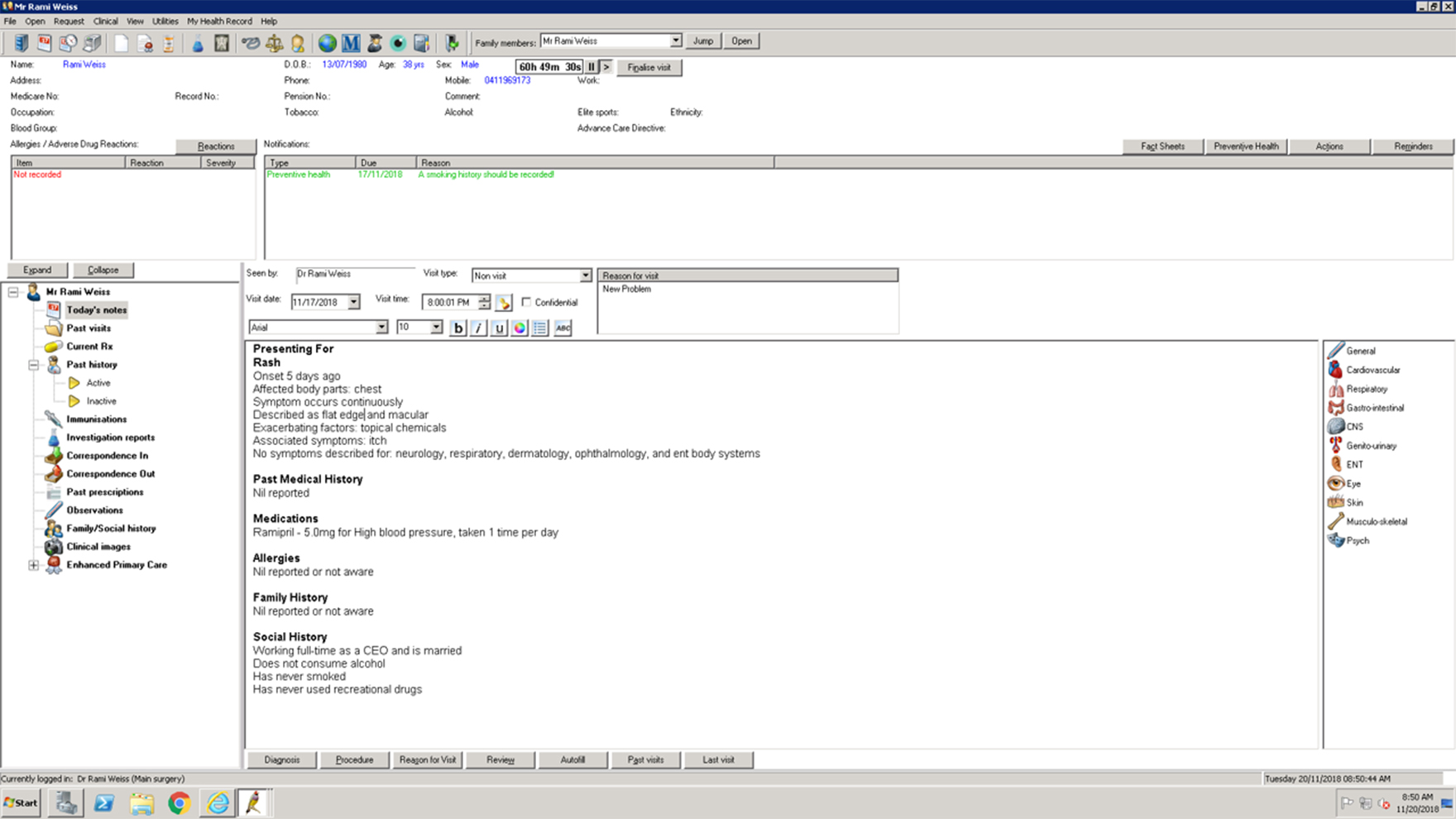
Rami Weiss – CEO, Healthshare
Doctors feel more rushed than ever, and are swamped by never-ending paper work. “They have lost control of their consultations because they don’t know why the patient is coming to see them before the patient walks in,” said Mr Weiss.
“We think we can solve this. Our product is called Better Consult. It’s a pre-consultation clinical questionnaire that the patient fills out before seeing their doctor.”
Essentially, the patient gets a text message a day before their GP visit that directs them to a secure questionnaire. Prompted by automated questions, the patient can disclose information about their symptoms, including duration, intensity, exacerbations, triggers, and so on. The patient can fill in their medical history, allergies, medications, social history, smoking status, or skip questions.
When the patient arrives at the clinic, the GP simply opens up their clinical software and reads a plain text summary of what is troubling the patient. “We are just getting started,” said Mr Weiss. “We have all these awesome features that we are building. So we’ll allow you to take a picture of your medication pack and convert it into the actual medication you’re taking. We’ve got multiple language capabilities we’ve built out.”

Silvia Pfeiffer, PhD – Founder & CEO, Coviu Global
Coviu is a start-up spun out of CSIRO that is looking to transform telehealth. The company has already launched a fast, secure video platform for doctors. What differentiates this from services like Skype or Zoom is that the software creates a digital waiting room that ensures doctors can manage work flow and aren’t interrupted during a consult. Around 2000 clinicians around Australia have signed up to the service. The company’s “superpower”, however, was to bring an extra magic to video consultations that made the experience almost better than being there in person, said Dr Pfeiffer.
The video consultation with a physiotherapist, for example, overlays an algorithm that calculates the patient’s range of motion when flexing and extending their leg muscles, providing an extra piece of quantitative information. The reason this is such an important tool is because more patients are undergoing knee replacements than ever in Australia, and patients are spending more time in hospital for rehabilitation because doctors want to ensure the patient is doing all the exercises correctly.
The solution was to bring physiotherapy to patients in the community, but this wasn’t easy in a country like Australia where there were so many remote and regional areas. Video consultations could be the answer, Dr Pfeiffer said. “In a live video consult you have a tool that helps the physiotherapy keep track of the progress of the patient. So every two degrees of progress matter and needs to be kept track of – that is what the algorithm does.”
The potential cost savings were huge; telehealth for knee rehabilitation could save “up to a billion dollars and free about 60,000 hospital beds every year”.

Dr Nishanth Krishnananthan & Dr Vijay Paul – Co-founders, Vantari VR
Medical imaging hasn’t evolved in over 30 years and the traditional 2D scan continues to be a problem for surgical planning, for medical education training and finally for patient consults. Vantari VR modernises imaging by rendering any patient CT or MRI scan in 3D.
“Imagine no longer having to see your patient as a 2D black and white slice,” said Dr Krishnananthan. Instead, clinicians can wear a headset and see everything in 3D.
“Our first application is for surgical planning,” said Dr Krishnananthan. “We’ve found with our preliminary data that VR not only reduces planning time by 40%, we also decrease adverse outcomes from surgery by 10%.”
The second application is medical training. “Through training scenarios with Westmead Hospital we’ve already found that 60% of students and trainees found learning and training in VR better than using mannequins,” Dr Krishnananthan said. The final application is VR to help patients better understand their health condition, which is being trialled in a pilot study at Campbelltown Private Hospital.

Catherine Resick – Founder & CEO, KinChip Systems
“Imagine if you always understood the best way to support your family and had all the resources you needed to do it,” said Ms Resick. That’s the dream that KinChip Systems is making a reality for the family members of people with complex needs.
“Navigating your way around the healthcare system can be incredibly challenging, very difficult and highly stressful,” said Ms Resick. “It’s not always easy to find the right services at the right time when you need it.” What consumer-centred care looks like at the moment is an array of fragmented portals, “each wanting to be the single source of truth but each ultimately expecting the consumer to engage with something different every time”.
These portals have a clinical focus and ignore many of the social determinants of health. KinChip Systems is a platform that provides one place for families to store health, education and personal information and to be able to securely share that with anyone in the care team. “Because we take a consumer-centred approach we bypass those institutional challenges about data sharing and collaboration,” said Ms Resick.
“To give you an idea of what that looks like, we make the platform highly engaging and a place where families can record important milestones in a Facebook-friendly way but it’s private and secure with only the people you want to share it with.” The platform produces a range of outputs, like a traditional health summary and vaccination schedules, and patients can customise what information they want to share and with whom they want to share it. “We’ve also structured this so that you can manage more than one family at the same time so typically elderly parent alongside children,” Ms Resick said.
“And there’s a resource directory so that families don’t have to rely on Dr Google for all their information. They can look at trusted resources with quality information to give them the information they need at the right time.”

Dr Robert Laidlaw – Founder & Executive Director, Secure Health Chain
Three doctors based in Wollongong, NSW, have jumped into the health blockchain market by launching a start-up called Secure Health Chain. Blockchain is a distributed ledger of digital transactions most commonly associated with the cryptocurrency bitcoin.
Many entrepreneurs have spotted the potential applications of blockchain in healthcare, and now the race is on to create the best product. Blockchain might be the technology that allows hospitals, primary carers and specialists to share health information securely, with absolute certainty that the information is accurate and being shared with a trusted party.
Dr Laidlaw said it was not necessary to understand how blockchain worked from a technical perspective in order to appreciate what the technology has to offer.
“Blockchain is like a digital fingerprint,” he said. “The issue in health is that the data is in silos and it is not connected in any meaningful way. Blockchain creates trust and verification for all interactions that we have. We’ll have a single source of truth where ever and whenever it’s needed.” Secure Health Chain’s proof of concept will launch in Wollongong in January 2019.