The peak body wants members to pass on tips on how to survive in general practice, but supervisors themselves are under pressure.
If primary healthcare is to be sustainable, showing trainees how to reduce the chances of experiencing burnout must form part of the supervisor’s role, said the profession’s peak body.
According to the General Practice Supervisors Association (GPSA), the group’s annual national survey “suggests a role for GPSA and training practices to support the wellbeing and self-care of the GP workforce, perhaps through targeted professional development activities which may have a protective benefits”.
“Understanding how to best support doctors to practise self-care, and to model those behaviours for junior doctors, is vital for safeguarding the sustainability of the primary health system,” GPSA chief executive officer Carla Taylor said.
“These results highlight the importance of GPSA and GPRA’s roles in raising awareness and facilitating a nurturing, supportive culture as a key component of best practice in this sector.”
But modelling these behaviours may prove challenging, given that 70% of the supervisors who responded to the survey reported that they themselves had experienced high levels of burnout.
The annual survey investigated the perspectives of GPSA members on their wellbeing and experiences in the previous 12 months.
In total, 319 GPSA members responded to the association’s survey during March and April 2022, with both males and females equally represented. 91% of respondents were GP supervisors and 88% were RACGP members. In addition, 66% were aged between 45 and 64 years, while 29% were based in NSW, 24% in Victoria and 22% in Queensland. 88% were working in community general practice.
While GP training will undergo a significant change in February next year, with the transition to college-led training and the disappearance of the RTOs, many supervisors may end up staying the distance.
More than half of respondents intend to continue GP supervision for the next 5 years, while 29.5% will stop within the next 5 years, 5% will not supervise in the future and 12% are unsure, according to the survey.
The location of the training practice – whether in a metro, rural, regional or remote site – did not appear to affect supervisors’ intentions.
The survey’s results also suggest a high level of satisfaction with RTOs, with 45% of respondents satisfied and 21% very satisfied with their organisation.
These findings, however, may not reflect the views of GP supervisors more broadly, with the GPSA cautioning that fewer than 10% of members responded to the poll.
According to the GPSA, supervisors who feel well supported in their workplace, avoid working when unwell, are engaged in professional development and look after themselves have lower levels of burnout and are more likely to remain in GP training for the next five years.
“What we need to focus on are the opportunities our findings speak to,” Ms Taylor said.
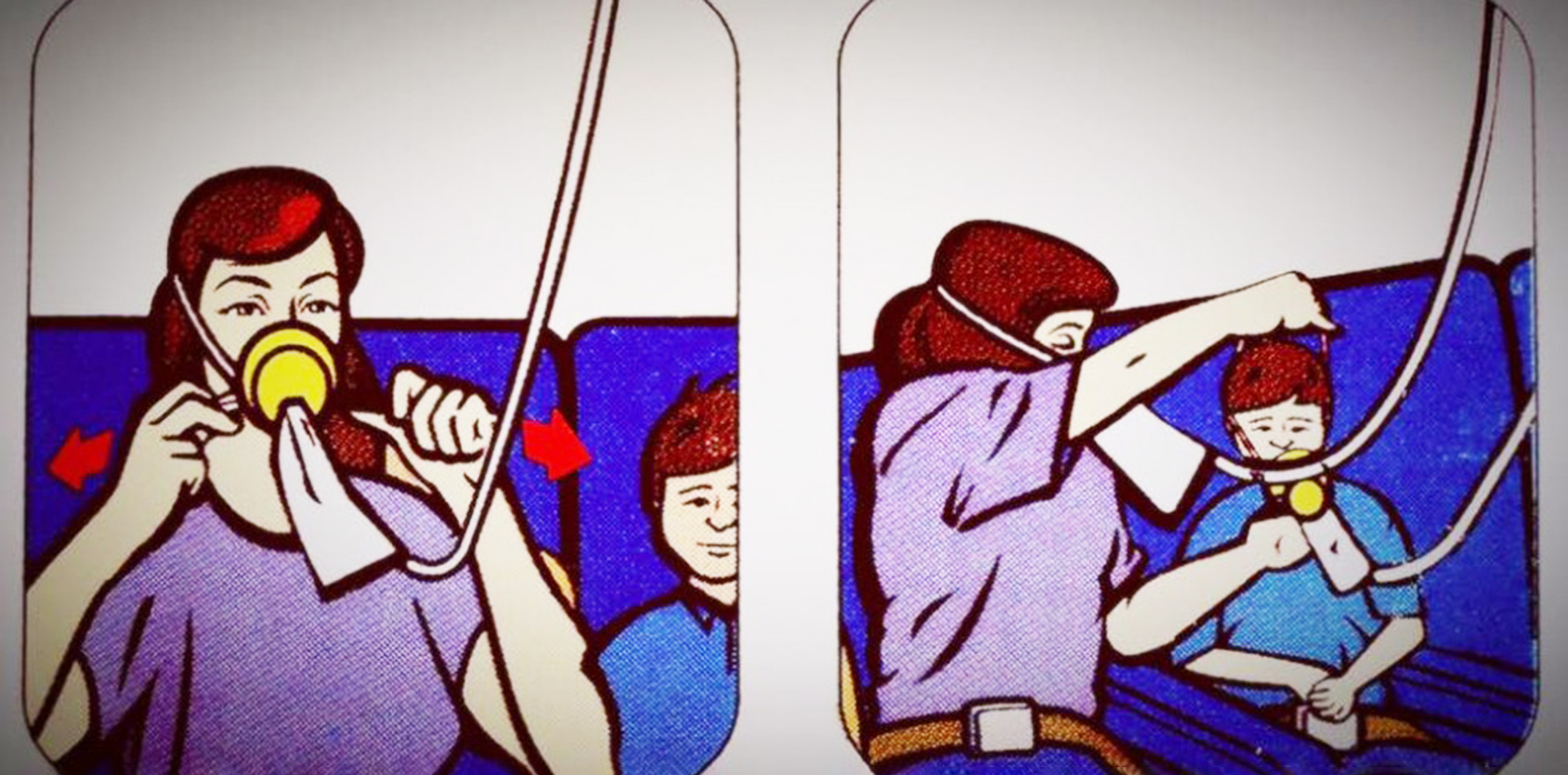
“Now is the time to do more to normalise and support self-care in general practice, to remind these individuals who underpin this nation’s healthcare that they need to apply their own oxygen mask first.”
Since 2018, the number of people applying for GP specialist training has continued to stay low, the workforce shortage has become painfully apparent in rural areas and knock-on effects of the pandemic have increased financial pressure on practices.
By 2032, the shortfall in GPs is predicted to number around 11,000.