Chronic pain may deplete the neurotransmitters that regulate negative emotions.
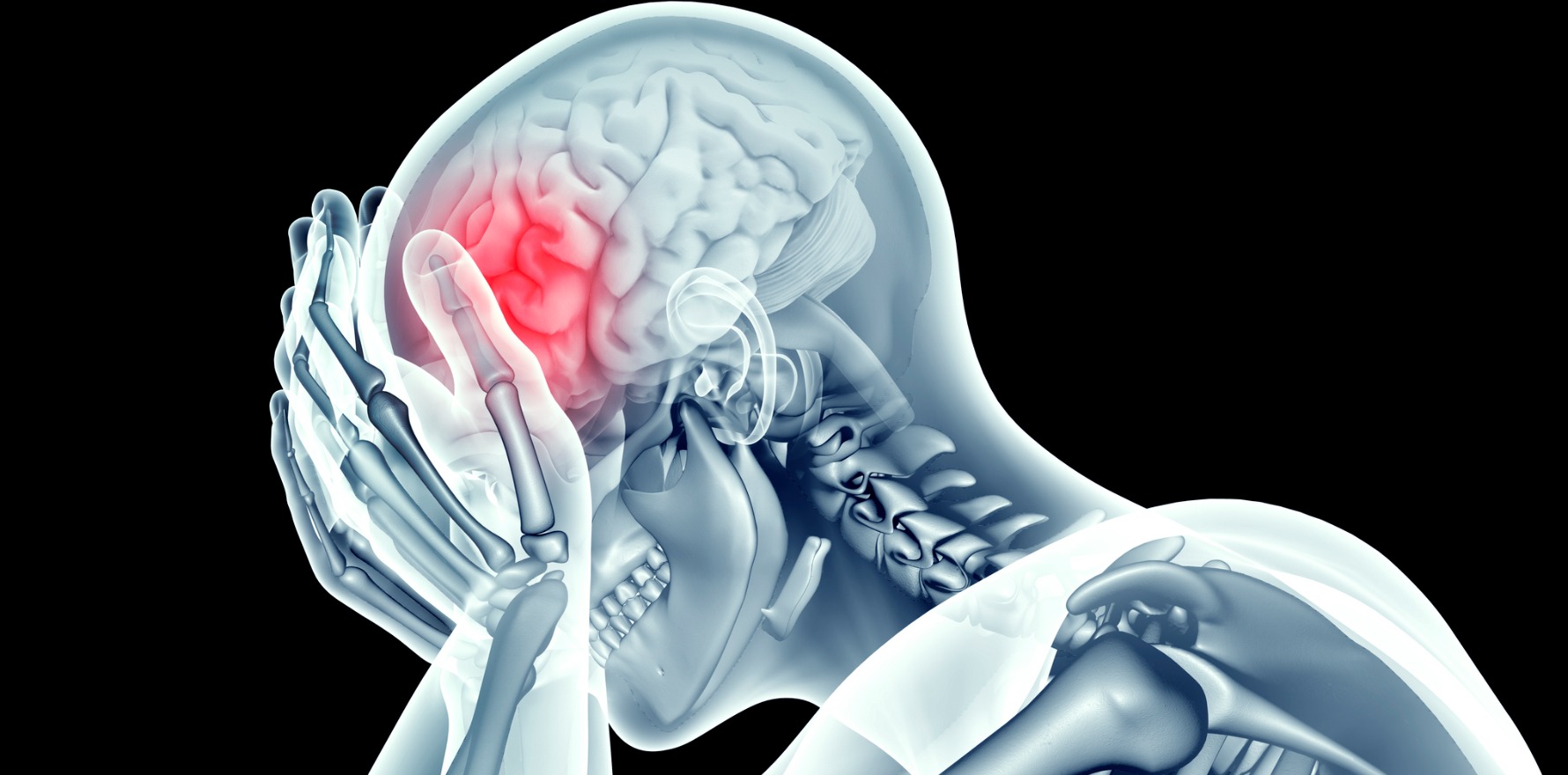
People with chronic pain have an imbalance of neurotransmitters in the medial prefrontal cortex, a part of the brain that sits right behind the forehead and is responsible for regulating emotions.
This imbalance may be caused by persistent pain and could be making it harder for chronic-pain patients to keep negative emotions in check, according to a study led by the University of NSW and the NeuRA research institute.
The findings, published recently in the European Journal of Pain, could help patients understand why they might struggle with low mood and offer hope for new targeted strategies and treatments, said Associate Professor Sylvia Gustin, a neuroscientist and psychologist at UNSW and NeuRA, and author of the study.
“People with chronic pain are often stigmatised for feeling depressed and unhappy. But chronic pain is much more than an awful sensation – it affects our emotions, it affects our feelings, it affects our personality,” she said.
Neurotransmitters facilitate and balance communication between brain cells. GABA, or gamma-aminobutyric acid, is the primary inhibitory neurotransmitter in the medial prefrontal cortex, and its role is to help dampen negative emotions.
In a cross-sectional study, the research team recruited 48 participants. Of these, half suffered from chronic pain. They scanned participants’ brains and looked at their medial prefrontal cortex to measure GABA levels.
The researchers found significantly lower levels of GABA in participants with chronic pain compared with the control group. The pattern was consistent regardless of the type of chronic pain.
“A decrease in GABA means that brain cells no longer communicate to one another properly, and feelings, particularly negative feelings, get amplified,” Professor Gustin said.
The relatively small sample size might be a limitation of the study. Nevertheless, Professor Gustin said, the study had clearly shown a difference between the two groups.
GABA was not the only neurotransmitter in the medial prefrontal cortex behaving differently in people with persistent pain.
In a previous study, Professor Gustin and her team found that levels of glutamate, another key neurotransmitter responsible for emotional regulation in the same region of the brain, were also lower in people with chronic pain. Decreased glutamate levels were linked to increased feelings of fear, worry and negative thinking.
“Glutamate can be a very toxic neurotransmitter,” she said. “The two studies give the big picture of what’s going on – it really looks like the way the brain cells are talking with each other is disrupted in chronic pain.”
Currently, there is no medication available for chronic pain that targets the medial prefrontal cortex. Pain drugs act on the central nervous system, leading to severe side effects, including dependence.
Professor Gustin said this study provided the ground for developing new, targeted pharmaceutical and non-pharmaceutical treatments.
Her team had developed an online emotional recovery program to help patients increase their capacity to regulate negative emotions.
“It’s not a psychotherapy intervention. The aim is to teach the brain cells to talk to each other properly again. That provides patients with the skills to self-regulate their negative emotions.”
The team welcomes patients interested in learning more about the program and can be contacted at neurorecoveryresearch@unsw.edu.au.