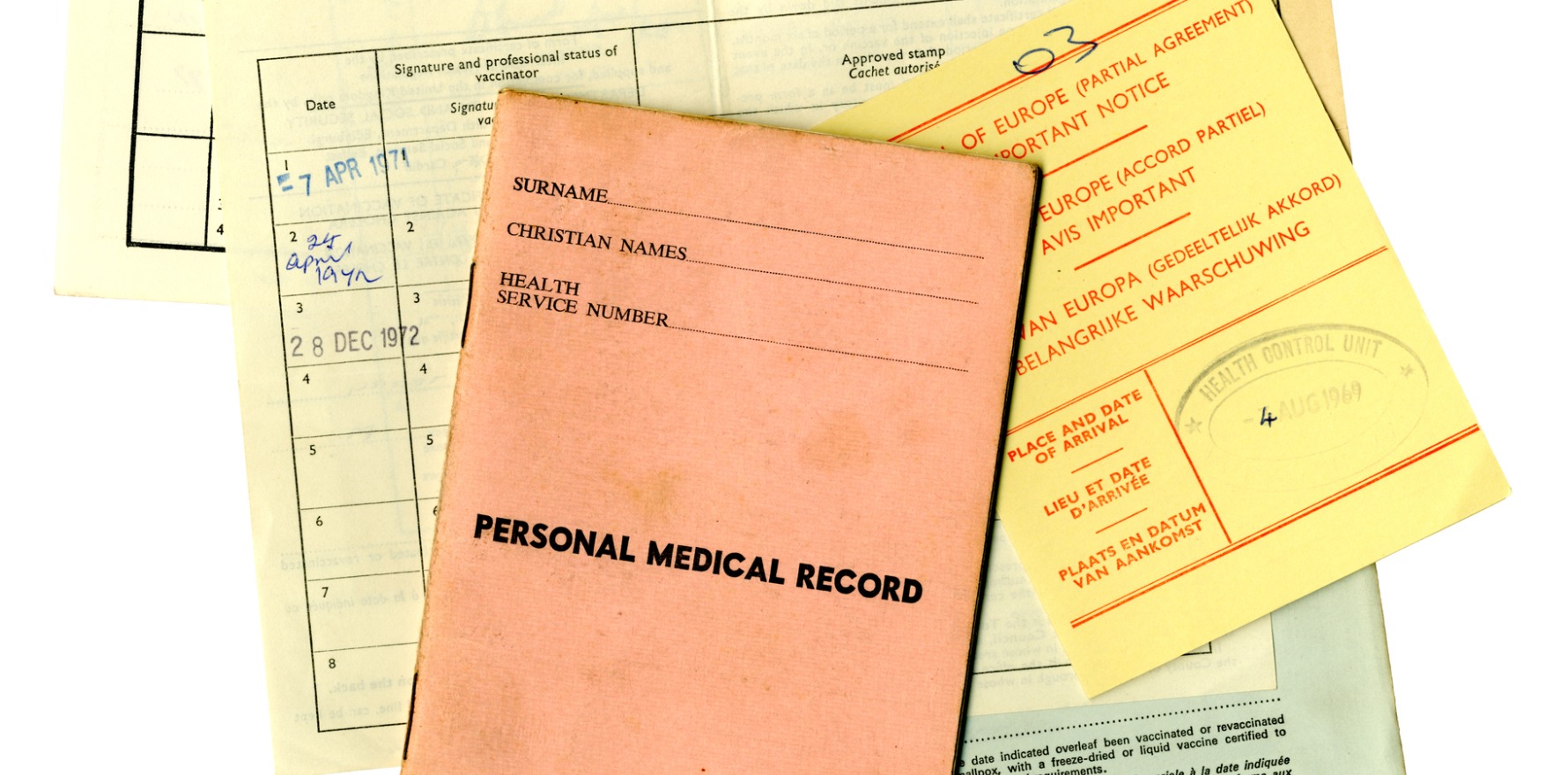
Practice management systems are unfit for purpose with health assessments forms that are ageing – like the population.
The holy grail of research is implementing evidence-based practice, but most general practice patient management systems draw on decades-old evidence, says frailty expert Dr Chris Bollen.
Dr Bollen is a GP and director at BPM Consulting where he delivers clinician workshops on understanding and treating frailty. He recently worked with Gold Coast PHN and Hunter New England and Central PHN to deliver an RACGP-accredited audit program to improving the Health Assessment for people aged 75 years and older.
He said that most doctors were unable to access up-to-date health assessment forms in their PMS for use in consultations with ageing and frail patients.
“The PMSs don’t have any frailty screening templates at all. Doctors are using their patient management software, and the health assessments do not have anything that discusses frailty,” said Dr Bollen.
“It’s very clear from the GPs’ feedback that they would like their software to keep up to date with evidence-based care.”
New clinical evidence, such as that on nutrition and exercise, are central to the prevention and management of frailty, he said. Despite this, the clinical evidence for ageing and frail patients in most Australian PMSs is around 25 years old, Dr Bollen said.
“This ‘dumb software’ still uses clinical templates from 1999, which was when the MBS introduced rebates for enhanced primary care plans.
“The gaps are huge between what is required in 2023 and beyond, compared to 1999. This impacts what is done, or not done, to support older people to live well and independently at home,” Dr Bollen said.
Dr Bollen said the population of Australia is “getting older every moment we sleep” and that many older people are struggling to stay well at home.
“It’s a matter of urgency. We need to be able to see a lot more older people and do it well. Our software should be helping us keep up-to-date,” he said.
“Many of our nurses and GPs have not had adequate training in the care of older people and require the software to assist them in what is required in an assessment. Software vendors are not doing enough to bring the latest evidence into everyday clinical practice,” he said.
TMR approached the two dominant primary care PMS providers for comment.
Best Practice
Danielle Bancroft, chief product officer at Best Practice said age of health assessment forms had been “acknowledged and discussed as an industry issue”.
She said that Best Practice and other vendors are working on the priority problem through the CSIRO and HL7 primary care working group.
Technically, the group is moving the industry towards interoperability by creating standardised frameworks and data consistency for health assessment forms.
The RACGP and National Aboriginal Community Controlled Health Organisation (NACCHO) have been collaborating on the first use case – Aboriginal and Torres Strait Islander Health Check Assessment (formerly MBS 715).
The technology underpinning the forms update can be implemented once by the vendor, but then reused for any health assessment form, Ms Bancroft said.
Ms Bancroft said that over the next 12 months BP will incorporate updated health check guidelines from the NACCHO-RACGP partnership and there are plans for pilot implementations. Best Practice updated the various Aboriginal and Torres Strait Islander health check forms in 2019.
“A number [of our health assessment forms] have existed for some time. Others are more recent, and in 2019 a number of them were updated,” Ms Bancroft said.
MedicalDirector – owned by Telstra Health
A Telstra Health spokesperson said MedicalDirector had a range of clinically developed health assessment templates available, but that they were intended to be adapted by healthcare providers and practices.
“We’ve found that practices prefer to develop their health assessment templates in partnership with their local PHN to address areas of focus for their particular region,” they said.
The Telstra Health spokesperson said that GPs could import templates relevant to them from PHNs, states and territories, and member organisations such as RACGP and AAPM. Both sources are able to be adapted in the MedicalDirector software.
Nevertheless, GP Dr Bollen said Australia’s PMSs for primary care were “clearly not fit for purpose”.
“The Royal Commission into Aged Care has many statements about those working with older people needing to have adequate training and they need to have adequate support, whether they work in community or in aged care facilities.
“From a system of care perspective, software has a part to play here,” Dr Bollen said.