Two in five trainees disagree or strongly disagree that exam feedback is useful and only a third are clear on what their fees are spent on.
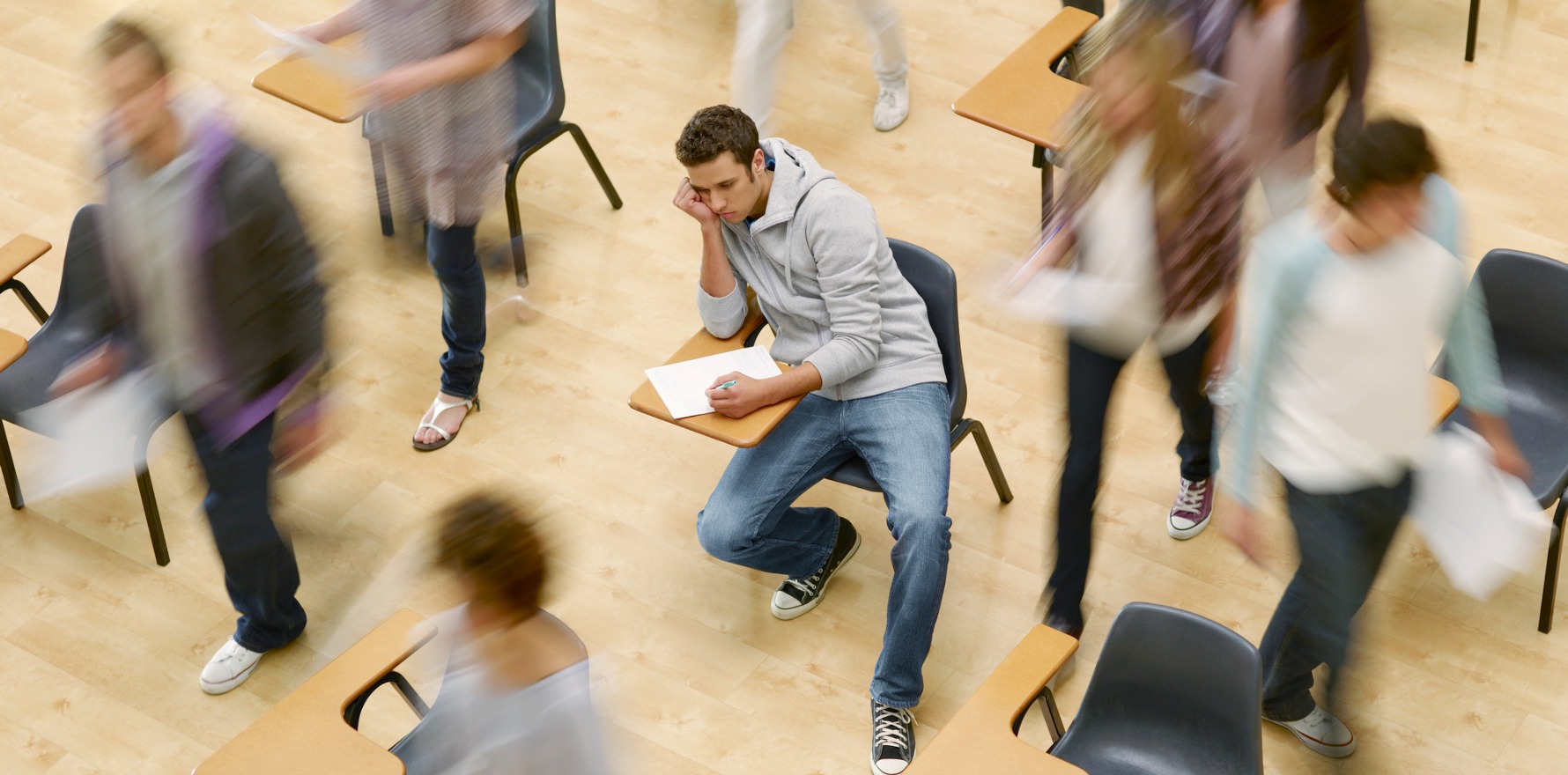
Exam feedback, or the lack thereof, and fees are causing trainee headaches, according to this year’s training survey.
Today, the Medical Board released the 2024 Medical Training Survey, detailing the experiences of nearly 25,000 medical trainees, over half of all doctors in training.
Of the specialist GP trainees surveyed – 3289 in total – 83% were training with the RACGP, 18% with ACRRM and 1% at the Australasian College for Emergency Medicine.
While feelings towards the relevance of GP training programs remained largely positive, the lack of exam feedback has been a consistent sticking point for doctors across all specialties.
According to this year’s survey, two in five trainees disagree or strongly disagree that exam feedback was useful (36%) or timely (41%).
For specialist GPs in training, 42% felt that they received useful feedback about their exams and 44% thought the feedback was timely, a minimal improvement on the average across all trainees.
Another pain point: fees.
Just over half of all specialist GPs in training – 51% — felt that the cost of the training program led to stress.
Only 37% agreed that the college provided clear information about how fees were spent and 20% felt that the cost of their training program was a barrier to progression.
The survey also found pervasive experiences of bullying, discrimination, harassment, sexual harassment and racism among trainees.
According to the survey, one third of all trainees experienced and/or witnessed bullying, discrimination, harassment, sexual harassment and/or racism, spiking to 54% of Aboriginal and Torres Strait Islander trainees.
Chair of the Medical Board of Australia Dr Anne Tonkin said that there was nuance within this data.
“The source of reported unprofessional behaviour varies between groups of trainees,” she said.
“For GP trainees (49%) and interns (54%), patients and their families were the most common source of unprofessional behaviour, anchoring deficits in the culture of medicine firmly in the context of wider community attitudes and behaviours.
“With robust evidence generated by trainees in the [survey], comes knowledge and the ability to develop effective strategies for change.
“MTS results anchor deficits in the culture of medicine firmly to wider community attitudes and behaviours.”
According to the survey, 63% of specialist GPs in training agreed that there were safe ways to raise wellbeing concerns and 53% felt that they were provided with psychological or mental health support.
The AMA called on institutions and employers to commit to the Every Doctor Every Setting Framework.
Related
AMA president Dr Danielle McMullen said the association was disappointed and alarmed at the survey results.
“This survey should be a major wake-up call to tackle the systemic issues that impact the training experience and wellbeing of doctors in training,” said Dr McMullen.
“We are disappointed doctors in training are still experiencing racism and sexual harassment, and we are particularly alarmed that 19% of all doctors in training are considering a career outside of medicine.
“Doctors in training are the future of our profession and we must ensure their training experiences are valuable and enjoyable so we do not lose their talent to other professions.”
AMA Council of Doctors in Training Chair Dr Sanjay Hettige said improvements must be made.
“It is appalling to see in this survey that 38% of Aboriginal and Torres Strait Islander trainees experienced or witnessed racism — more than double the rate of non-Indigenous colleagues,” Dr Hettige said.
“While our medical training system continues to perform well in terms of education and a variety of other areas, there is still a long way to go to address some of these systemic and cultural issues.”