Tailored guidelines for general practice are lacking, but it seems GPs must arrange and pay for fit-testing themselves.
If you’re still confused over what personal protective equipment is best for everyday clinical practice, you’re not alone.
GPs in areas with active covid cases, despite being almost two years into the pandemic, remain confused about where to source appropriate PPE and whether they should be fit-tested for a N95 mask.
Instead, GPs are being left to decipher difficult PPE guidance from their local health districts, such as the following chart which was recently circulated to healthcare workers on social media.
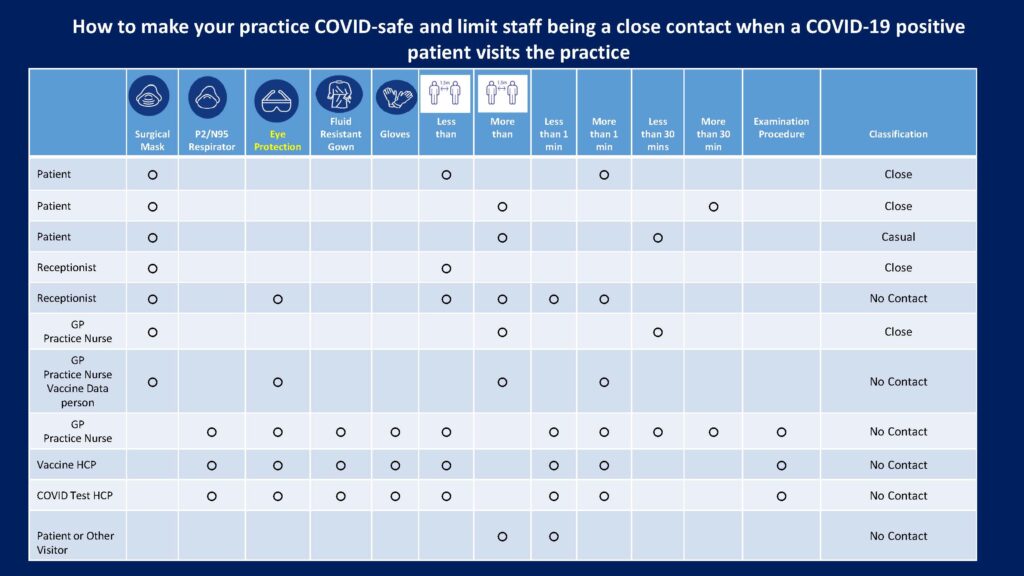
Does that make it any clearer? No, we didn’t think so.
TMR put a series of questions to the Department of Health and the RACGP to try and make it a little easier for primary care to understand the official PPE advice and how practices could go about organising professional fit-testing.
“Our understanding of the transmission characteristics of SARS-CoV-2 has evolved since the commencement of the pandemic with emergence of new evidence and the evolution of more transmissible variants,” a DoH representative told TMR.
“It is becoming increasingly clear that SARS-COV-2 can be transmitted through a range of potential routes ranging from smaller particles (aerosols), respiratory droplets, direct physical contact with an infected individual, and indirectly through contaminated objects and surfaces.”
But the official guidance for PPE use in healthcare settings, introduced in June 2021, offers an eight-page explanation of how workers might go about assessing their covid risk and adopting various protocols.
Last month, the National Covid-19 Clinical Evidence Taskforce (NCCET) published a much more succinct decision tree based on local risk factors.
In a nutshell, if you’re working in an environment where there is high risk of transmission, P2/N95 respirators are preferred to face masks, along with other PPE such as eye protection.
But the advice stipulates that healthcare workers who wear P2/N95 respirators should complete fit-testing before first use and perform a fit (seal) check properly each time they are used.
According to the DoH’s advice, in situations where fit-testing has not yet been carried out, and a P2/N95 respirator is recommended for use, a fit check was still preferred to using a surgical mask.
For those who hadn’t had a fit-testing yet, which is probably most GPs, the RACGP has created a short video explaining how to carry out a seal check of an P2/N95 respirator.
Back in June TMR reported advice from the Infection Control Expert Group that all healthcare workers “providing direct patient care or working within the ‘patient/client/resident zone’ for individuals with suspected or confirmed covid should now have access to fit-tested P2/N95 respirators”.
It said respirators were preferred over surgical masks for “high-risk settings”. The NCCET said a local area being a covid hotspot made a setting high-risk.
When it comes to ordering PPE, practices in Commonwealth declared hotspots could do so through their PHN, where normal supply was not available. The supplies would be made available through the National Medical Stockpile.
RACGP president Dr Karen Price said she welcomed the Australian Government making PPE available to GPs in hotspot areas over the previous months.
“This is essential to protect GPs caring for patients on the frontline, and the RACGP has long been calling for it throughout the pandemic,” she told TMR.
In addition, Dr Price encouraged practices to contact their PHN to see if they could arrange access to PPE fit-testing.
“This should only be performed by an appropriately trained person,” she said.
“Some PHNs are supporting practices to access fit-testing in their local area. In the first instance, GPs should contact their local PHN for advice on how to access fit-testing.”
Dr Price said GPs could also find an accredited fit-testing provider through the Australian Institute of Occupational Hygienists program RESP-FIT.
But considering that a number of healthcare workers employed by state-based services were able to access fit-testing for free this year, it’s unlikely general practices would be thrilled about having to wear this expense themselves.
From what TMR can glean from the providers listed with RESP-FIT, testing starts at about $100 for every respirator fitting, with appointments lasting about 30 minutes each.



