The elephant in the general practice consulting room is Medicare wanting proof that it's getting value for money
There has been an enormous amount of comment about the 40 minutes-plus proposed change to item 721/723. I would like to run the whole concept through the iconic Australian “pub test”.
Let us assume that patients believe our medical ideology of the doctor-patient relationship. This is that it is a one-to-one relationship and that outside parties such as insurers (Medicare or health funds) should not have a significant say in what happens during the consultation. The aim of the medical consultation is to produce a health result which the patient wishes and is willing to pay for.
If the patient had to personally pay $258 ($144 for 721 and $114 for 723) the pub conversation would go like this: “I went to my doc for this care plan stuff. After seeing the nurse, I saw my doc. He spent same amount of time he usually spends with me, then he charged me $144 for these sheets of paper. It got worse. He then charged me $114 for a referral to my physio and podiatrist. The sheets he handed me were virtually same content as the first one but with a different name. So, I said: Nah! Not going to pay that, doc!”
This scenario will never eventuate, of course, because with bulk billing the price checking that would occur with the patient wanting value for his or her money does not happen. It is also politically impossible to dismantle this in general practice with both political parties trumpeting bulk billing rates of over 80% in GP land as a success. Therefore, we are left with the elephant in our consulting room; Medicare wanting value for money.
Initially, I must say, I believe that the Department of Health chronic disease management (CDM) process required of GPs was fatally flawed from the very start. What we got was a perfect bureaucratic approach to CDM. The primary function of the GP in the current scheme is to document all these problems/ goals/managements in a special way and give everyone lots of sheets of paper, and miraculously all CDM problems will be solved!
Documentation may work for government, but doctors are in the business of “doing” to improve health outcomes for patients, then as a secondary consideration documenting process. So, we GPs were forced to become bureaucrats, and we hated it.
My second contention is that GPs have been cynically exploited financially by both Labor and Coalition governments with the freeze on Medicare item numbers. This encouraged, in turn, a cynical approach to CDM by GPs: “OK, I will do this stupid bureaucratic paperwork and take the money to help subsidise my practice.”
Because patient-driven price checking is politically inconceivable, there are only three ways out of the mess:
(1) Abandon CDM item numbers completely and rely on the generosity of ordinary item number rebates.
(2) Introduce compulsory performance indicators for CDM, as in the UK, with their “quality outcomes frameworks” (and the onerous recording of same).
(3) Modify the current CDM process.
I believe the MBS Review committee meant well with its suggestions on CDM.
Essentially, what they said was: “Hey guys, you need to spend more time and take this seriously; and we are going to combine the 721/723 to reduce the amount of documentation you have to do.” Before you howl me down: No, I not agree that all care plans need to be 40 minutes plus. I think the logical solution is, as for mental health plans, there are 20 minutes plus and 40 minutes plus.
Is there any hope for CDM management? To give you an idea of what is possible I would like to tell you what we do for CDM in our general practice, Alexandra Park Medical Centre, Bundaberg, Queensland. Look up our website and see how well our PHN statistics compare with the average for our region.
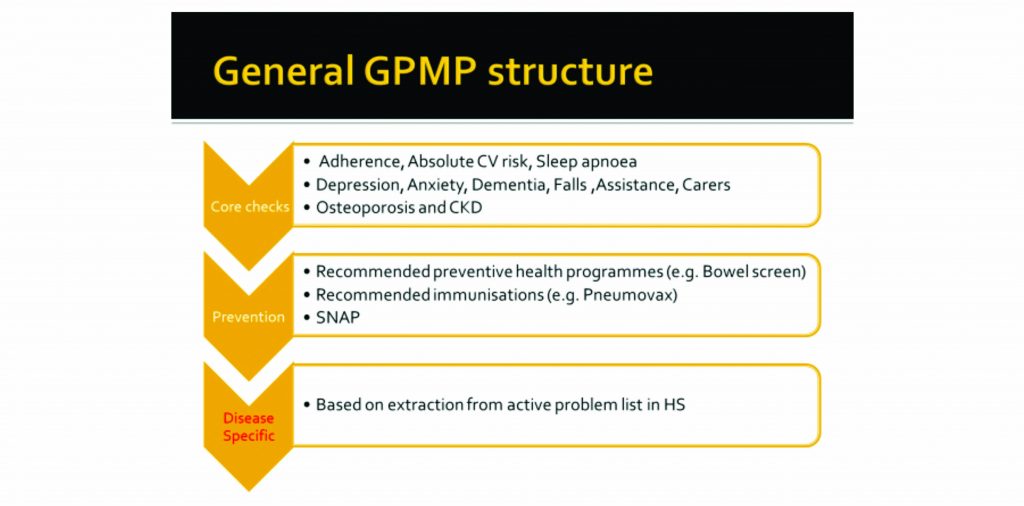
We have developed our own CDM software, Patient Assistance Tool (PAT) which works with Best Practice. We have just launched our PAT web-based version on our site, patsoftware.com.au. (See image below) We allocate 15 minutes each to the patient and nurse to do “core check” and “prevention” sections and 30 minutes to the doctor, so an hour in all. Our concept of the GPMP and TCA is to identify any actions that will be required over the next 12 months. It is not an attempt to solve everything in one go!
A good GPMP will generate good follow-up. For example, February 2019 Medicine Today reports that in patients over 65 years, only 50% have received pneumovax and only 10% pertussis. We certainly have generated a lot of follow up immunisations for our nurse.
A number of doctors have talked about knowing their patients well, these are the “known knowns”. There are also ‘‘unknown unknowns”, and our practice endeavours to find these as well.
A good example is chronic kidney disease (CKD). In a March AJGP article, it is said that only 20% of patients with CKD had a diagnosis documented and only 25% of patients with CKD have the appropriate monitoring. PAT automatically extracts the latest eGFR and microalbumin for the CKD question and has an education icon which links to the CKD site for clarification of CKD stages and the monitoring required.
Medicare requires that a comprehensive plan must describe the health care needs and problems. It does not say SOME of them! So, we review ALL the current active problems and update the whole health summary. This is where “knowing the patient” comes in, hence, I believe, only GPs can do this section, not the nurse. We do a medication review and print out the due scripts at this stage.
PAT extracts all active diagnoses from our records system [Best Practice] and adds specific extra questions for any of the 33 common conditions present. This is used to plan future action. Each disease specific question has an education link icon, which when clicked on takes the doctor to the latest guideline on that condition. e.g. Coeliac Australia for its recommended annual check for coeliacs. Similarly, for androgen deficiency, and other less common conditions, as well as the common chronic diseases.
PAT specifically checks for skin cancers and melanomas in the history and suggests a reminder be added for skin check. Performing these we have found this has substantially increased our skin cancer surgery rate.
In the editable plan at the end, PAT displays the total time taken so far for all stages (just as BP does in your consultation).
I believe that if we take GPMPs and TCAs more seriously, and spend more doctor time, we will reconnect with our ‘doing” role.
We can achieve the “Three Goods” rule:
Good for the patients (more and relevant care).
Good for the doctor (practising up-to-date, relevant medicine and the spinoff of more services e.g. skin surgery).
Good for the government (increased participation in preventive activities and immunisations).
Dr Pat Byrnes was national RACGP GP of the year in 2010, and is principal at Alexandra Park Medical Centre, which was the national RACGP practice of the year in 2006