In Queensland, one terminally ill patient takes their life every four days. The state election could determine whether voluntary assisted dying laws go to a vote.
Marj Lawrence watched the hardworking man she’d known and loved for decades fade away until there was little of him left.
The illness – myelodysplastic anaemia – that had crept up on Brian, a man who loved the land and took just one holiday in 40 years, would also claim him.
“In the end, he was just an absolute skeleton, he was like a rag doll,” Ms Lawrence says, speaking from her Townsville home. “I nursed him at home right up until his last breath, and after he died, I thought to myself ‘There has to be a better way to die than this’.”
The 83-year-old grandmother has watched six relatives die protracted deaths and she herself is battling pancreatic cancer.
“Three of my friends have died from pancreatic cancer in the last two years, and they all had terrible deaths,” she adds.
The drawn-out suffering she witnessed her friends and family go through pushed Ms Lawrence to become a fierce campaigner for voluntary assisted dying.
A year-long probe of public opinion in Queensland received thousands of submissions and found a majority of people were in favour of it.
That support wasn’t enough to convince the state government to introduce a law to parliament.
However, it did send laws drafted by two Queensland University of Technology professors and backed by the majority of a parliamentary committee to the Queensland Law Reform Commission for review.
Ms Lawrence says it is time for the state government to use its powers and give terminally ill patients a choice to die.
“If I end my own life without law, I’ll have to do it by myself,” she says. “But if I can work for a law to get into parliament, that will allow the family to be with me and probably doctors to make sure that nothing goes wrong.
“That’s why I’ve worked so hard to get this law.”
Officials within Premier Annastacia Palaszczuk’s government have told advocates they will bring the proposed law to a parliamentary vote if Queenslanders re-elect Labor at the October poll.
But those same campaigners are disappointed by its decision to push that vote into the next term of government, and say church leaders have met with the most senior MPs as a group to voice their opposition and exert pressure.
David Muir, chair of the Clem Jones Trust, is among the band of advocates meeting with voters in regional seats to promote the draft law and ensure they know which candidates stand for what.
The Liberal National Party’s position against voluntary assisted dying is well known, and there are real concerns legislation will be sidelined for years if the party seals an election win.
In that time, hundreds of terminally ill Queenslanders are likely to take their own lives.
If her disease progresses, Ms Lawrence vows she will be one of them.
“I don’t want to suffer, and I don’t want to go into a palliative care or nursing home, so I intend to end my life,” she tells The Medical Republic.
The former teacher worked out a plan for her death years ago and said her family speak freely about dying.
“We all know that Mum has the means to end her own life and in the back of my mind, my concern was always ‘When will she make that decision and how will she make that decision?” says Fay Edwards, one of her daughters.
“She’s made it very clear that she would still be talking to medical practitioners before that, and make sure that all options had been exhausted, and that we would be in those conversations.”
Ms Lawrence is the bedrock of her family, who say they want to be there for her when she decides her time has come.
“We don’t want her going on her own without family members there,” says Jenny Fisher, another of Ms Lawrence’s daughters.
“We’d be very, very sad about that.”
There is currently no option to help terminally ill patients die in Queensland, and one patient takes their life every four days.
They must do it alone or risk their loved ones facing criminal charges for getting involved.
“You have to have no knowledge of what’s going to happen, or not be there, which is just very upsetting, that we wouldn’t have the opportunity to be there and support her, or just be there, so she’s not on her own,” Ms Edwards added.
Sid Finnigan, a retired ophthalmologist and Queensland convenor of Doctors for Assisted Dying Choice, has spent the past few years meeting with parliamentarians and speaking at public education forums.
He wants patients like Ms Lawrence to have more control over what happens to them when they reach the end-stages of their terminal disease.
“Every inquiry around the world has had the same evidence, that despite our best-intended palliative care, the fact is it doesn’t work for everyone,” Dr Finnigan said.
“Some people still have drawn-out deaths that they wouldn’t wish for themselves if they did have the legal, voluntary avenue with full safeguards.”
The Australian Medical Association, which represents a third of the nation’s doctors, does not believe they should be involved in interventions with the primary purpose being to end a person’s life.
However, the peak medical body doesn’t class treatments such as sedatives or painkillers that ultimately speed up the death of a dying patient as euthanasia.
Chris Moy, AMA Vice President, says there is a public conversation to be had about voluntary assisted dying; however, exemptions and protective legislation for doctors are critical, along with better funding for palliative and aged care.
“The function of whether somebody has a good death is more to do with government resources to provide people with a good death or not,” Dr Moy said.
Protections for doctors who provide pain relief that speeds the end for patients already close to death must be built into the law, he added.
Laws that contain versions of that circumstance, known as the double effect, have been introduced in South Australia, Queensland, Western Australia and the ACT. But Dr Moy, a South Australian GP, says more consistency is needed.
He also wants non-requirement laws that free doctors from having to provide treatments with no medical benefit for their patients.
“There’s this feeling sometimes that doctors can be compelled to provide treatment that is futile, and we need explicit legislation to say that we don’t,” Dr Moy said.
“You’re telling us on the one hand that you want to end your life, but on the other hand we get complained about for keeping on going when we shouldn’t be.”
Dr Moy argues that allowing voluntary assisted dying may shift the value people place on the lives of others and themselves and increase the risk of families pressuring their elderly to end their lives for financial and other gains.
“People can have their beliefs, but it has to be a societal decision as a whole because it has ramifications,” Dr Moy says.
He is calling on governments not to see the introduction of voluntary assisted dying as a solution for a chronically underfunded and under-resourced aged and palliative care sector.
He says passing voluntary assisted dying laws may solve an issue around when and how people could die, but does not solve ongoing issues within aged and palliative care.
“To some degree sometimes, it just feels that once people have had the debate about voluntary assisted dying, they feel the end of life is sorted out, and it hasn’t been – not even close,” Dr Moy says.
Though it is not up to the AMA to decide whether voluntary assisted dying becomes legalised, in states and territories that pass voluntary assisted dying laws, the AMA has a role to play drafting regulations for doctors and patients, he says.
“We have to be involved in setting up the protections, not only for doctors who do or don’t want to be involved, but we’ve got to make sure that the boundaries are such that we minimise the chance of coercion or that people start to devalue their own lives,” he says.

A poll by the AMA of its members in 2016 found half of the respondents didn’t think doctors should play a part in euthanasia or physician-assisted suicide, while 38 per cent said they should.
An Australian Doctor survey found half of the doctors it approached were in support of voluntary assisted dying.
Dr Finnigan and Melbourne GP Nick Carr, who has assisted patients in dying under Victoria’s legislation, says the cohort of doctors against the practice are cloaking their religious beliefs in arguments about slippery slopes and coercion, and putting their faith before their patients.
“I have absolutely no problem with people having an ethical or religious-based objection to voluntary assisted dying,” Dr Carr says.
“But if you have, come out and say that ‘It’s not for me and I don’t plan to work with it’ – do not then force that view on other people.”
Since laws passed in Victoria, a majority of patients who have begun the process have died from their illnesses before needing or getting access to the medication that would kill them.
Dr Carr has however set up a fatal IV infusion and been one of the last people in the room for a handful of terminally ill cancer, respiratory and cardiac patients who asked for help to end their lives.
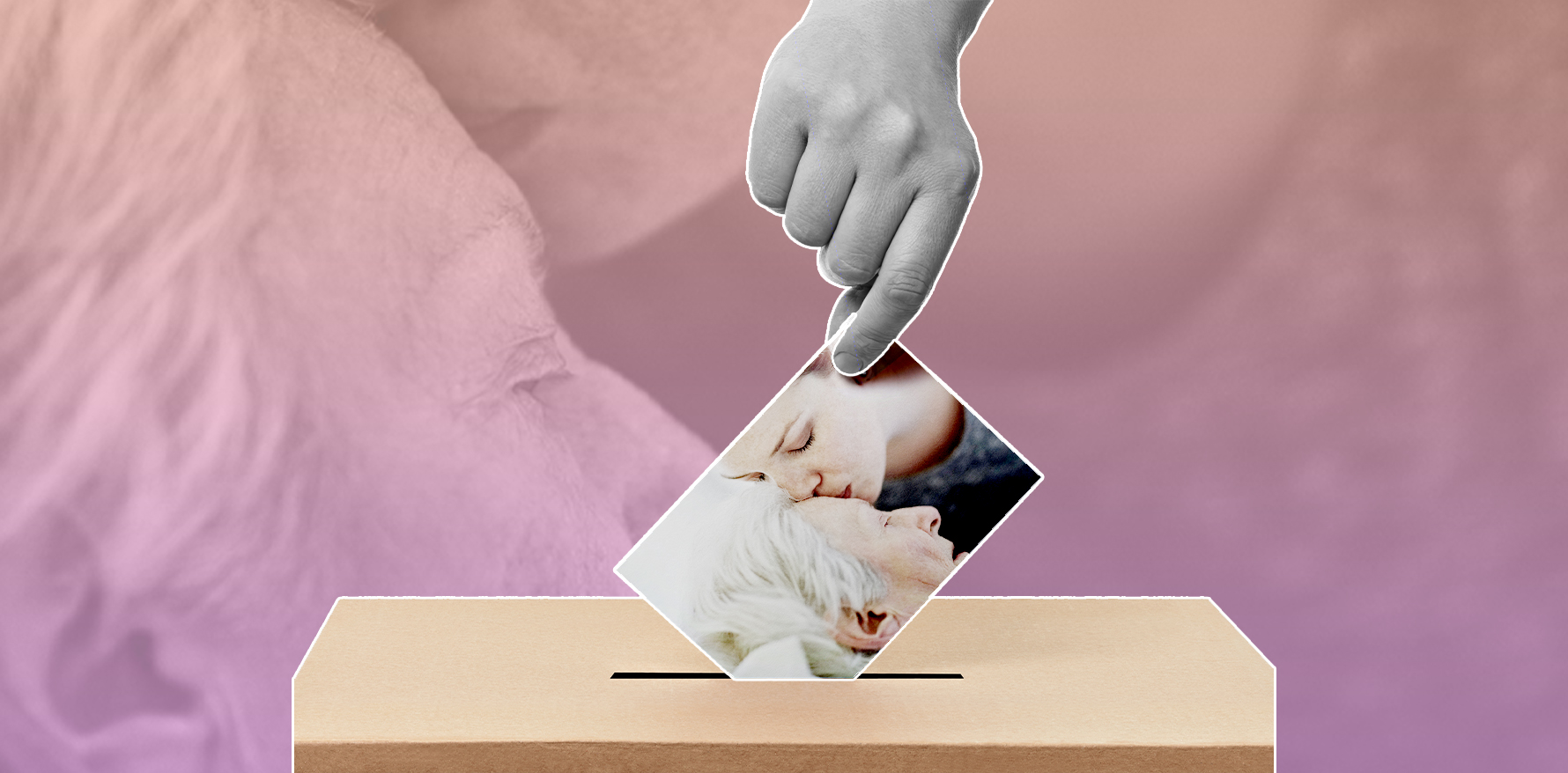
“I’ve been to a woman’s house where 12 relatives were crowded around her bed, taking the last photographs, kissing her goodbye, and then I asked them all to leave bar her husband while I put the drip in,” he recalls.
“She died very quietly, very peacefully with just me and her husband there, with all the rest of the relatives having said their goodbyes, waiting outside.
“It was one of the most gentle, beautiful experiences, incredibly moving, but it was from her point of view exactly what she wanted.”
He insists voluntary assisted dying, and better end-of-life care, are not mutually exclusive, and that the argument in favour of medical help to pass is about giving patients a choice.
“Everyone should have access to high-quality palliative care, but just putting money into palliative care will not relieve the suffering of this small group of people,” he says.
“For this group of people, the only way you’re going to relieve their suffering effectively is by providing them with a voluntary assisted dying option.”
Victoria’s legislation is viewed as the world’s safest and most safeguarded.
Doctors and advocates say it wouldn’t have passed parliament without restrictions such as prohibiting doctors from initiating the conversation about voluntary assisted dying, or the six-month and twelve-month prognosis limits.
It has resulted in some practical difficulties for doctors trying to estimate how long their patients could live, and there are concerns it is not accessible to less educated patients or those whose first language isn’t English.
“It’s certainly true that we are unhappy about the prohibition for doctors raising it with patients, because it’s ridiculous that something which is a patient’s legal right, that’s a medical procedure, we are banned from advising them,” Dr Carr says.
“It’s a little bit like saying if I was a cardiologist, I could tell people about medications they can take, but I can’t tell them about bypass surgery.”
The prohibition and prognosis safeguards were left out of Western Australia’s new law and was ditched by Professors Lindy Willmott and Ben White, who drafted the regulations now under review in Queensland.
“It’s a really, really hard job to draft a regime that allows access to voluntary assisted dying by people who should get access and at the same time havs sufficient safeguards so that vulnerable people are protected,” Professor Willmott says.
“Coming back to the Victorian legislation, one of the concerns that Ben and I had was that there are so many safeguards and the regime is so complex, that that might put up some barriers for people getting access.”
Under the Queensland draft, patients seeking voluntary assisted dying must have an incurable disease, which must be advanced, progressive and fatal.
The parliamentary committee that investigated the issue recommended there be no time limits on a person’s assisted death, and that those with a mental health illness should not have their access blocked, as long they can make decisions.
“Members of the community said the bill didn’t go far enough and wanted to be able to access voluntary assisted dying when they have dementia but no longer have the capacity to make those decisions, through directives laid out in advance,” Professor White adds.
“When they no longer recognise their family, and they can’t do things, and they’re sitting in a corner all day, they want assistance to die, but won’t be able to ask for it because they won’t have decision-making capacity.
“That was the main feedback, that they wished it went further.”
Marj Lawrence counts herself a lucky woman for the life she has lived and the family she has raised.
She says the prospect of being able to avoid the lengthy and painful deaths her loved ones experienced gives her comfort as she gets older.
“Knowing that I have control at the end of my life, I can’t tell you how much that is worth,” Ms Lawrence says.
“I think if we had a dying with dignity law, everybody would have access to that information, and they wouldn’t have to worry.”