Learn the risk factors for dry eye syndrome and why early treatment is important.
With around 1 in 5 adults affected by dry eye syndrome (DES)1 – are you aware of which patients are most likely to present with DES and the importance of early treatment?

Early detection and self-management with topical lubricants — such as MURINE® Dye eyes — provides important relief from uncomfortable symptoms and helps restore and maintain a stable tear film.1,2
What is DES?
Dry eye is characterised by a loss of homeostasis in the tear film – a unique three layered thin film that covers the outer mucosal surfaces of the eye.3 The key DES aetiologies being tear film instability, hyperosmolarity, ocular surface inflammation and damage.3,4
The two main subtypes of dry eye are3:
- Aqueous deficient dry eye – with reduced tear production
- Evaporative dry eye – commonly related to meibomian gland dysfunction5
Most patients with DES are now thought to have a combination of both subtypes.3
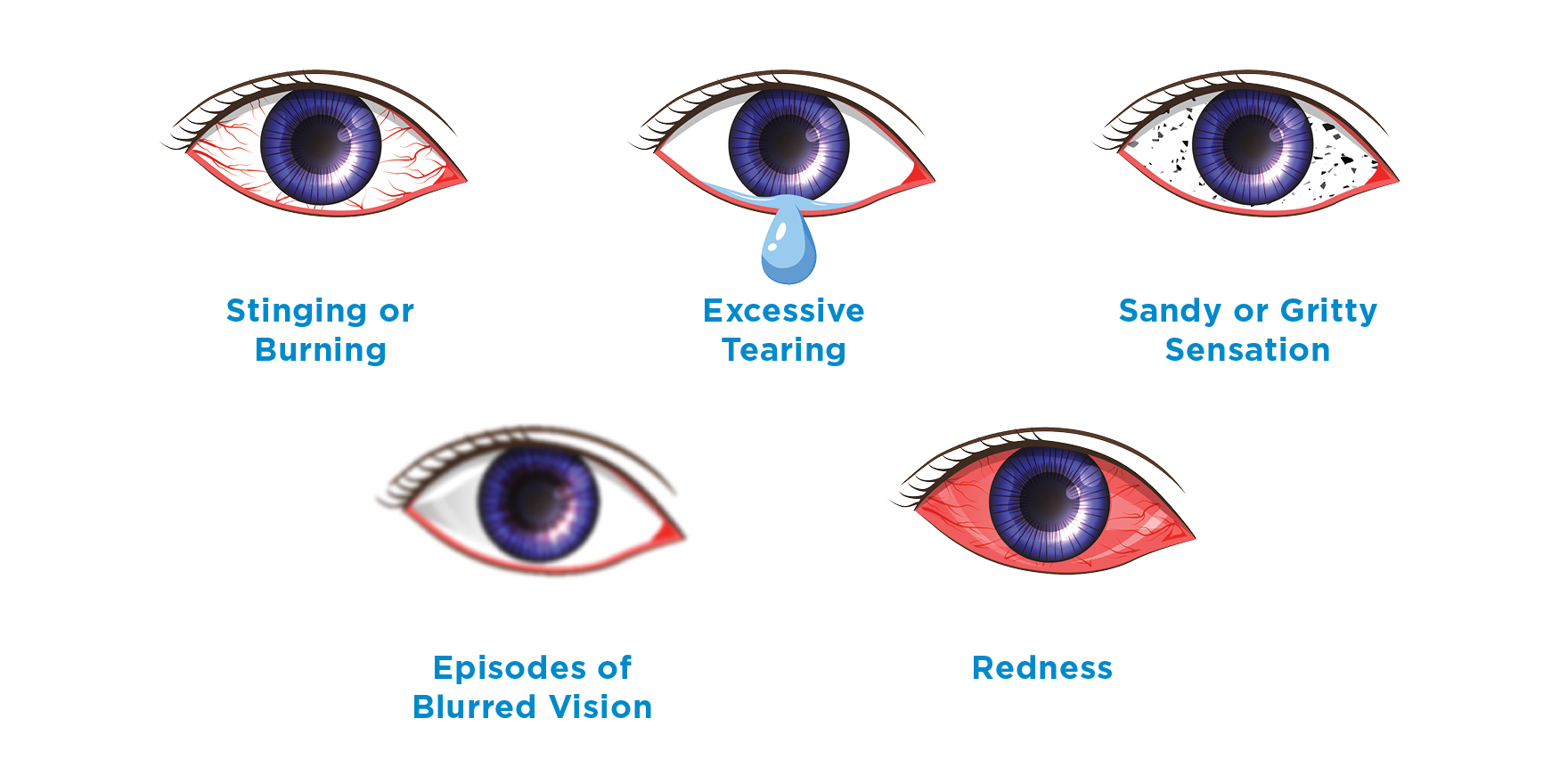
DES has a highly variable presentation, including burning or grittiness, pain or a foreign body sensation that gets worse during the course of the day.6,6 Vision can also be affected, and reflex tearing can occur, along with sensitivity to light and redness.1,6
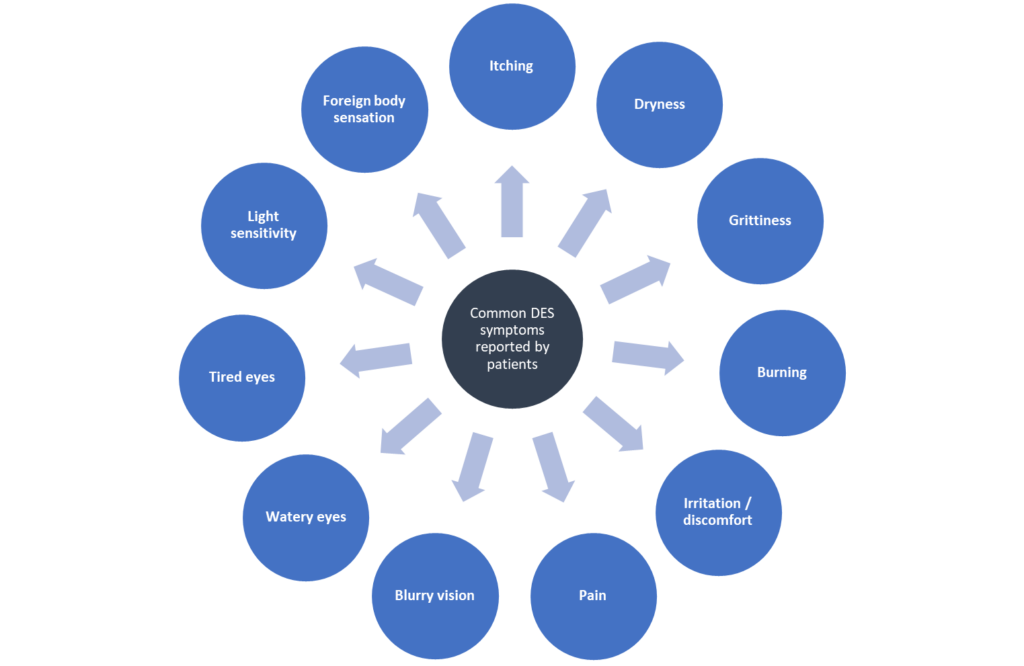
Patient-reported symptoms in dry eye syndrome (DES).6
Who gets DES?
DES risk factors can be systemic (ageing, other health conditions), intrinsic to the eye (topical medications, wearing contact lens), or environmental factors (computer use, air pollution).7,8
Many of the patients seen in general practice may have one or more DES risk factors, including:
The older patient
Older adults are susceptible to:
- Inadequate tear production – due to lacrimal gland dysfunction, altered reflex secretion, diminished corneal sensation or inflammatory destruction of lacrimal glands.9
- Meibomian gland dysfunction – linked to cutaneous hyperkeratinisation and narrowing of the meibomian gland opening, or reduced quantity/quality of the lipid-rich meibum that helps stabilise the tear film and prevent evaporation.10
Other age-related risk factors include polypharmacy, androgen deficiency, decreased blink rates, inflammatory systemic conditions and oxidative stress.9
Even seemingly benign DES vision impairment can further impair naturally deteriorating vision. Early DES screening and prompt treatment can make a difference to the older patient’s mental health, self-confidence and daily functioning.9
The patient with diabetes
DES prevalence in patients with type 2 diabetes can be as high as 54%,11 while over half of patients with either diabetes or borderline diabetes may report clinically relevant dry eyes – even a family history of diabetes may lead to an increased tendency to DES.12
Diabetes can lead to reduced corneal sensitivity and reduced blink rate with increased tear evaporation, and reduced tear production.13
Patients with longstanding diabetes may report fewer DES symptoms and it is important to be aware that this group of patients may not seek care early.13
The menopausal patient
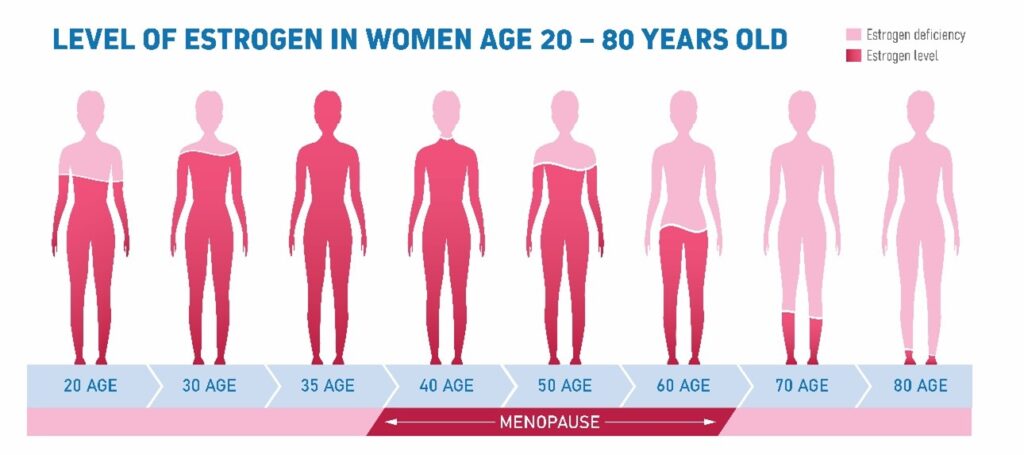
Did you know an estimated 61% of women transitioning through menopause display dry eye symptoms?14
The role menopause plays in DES is not fully known, but both meibomian and lacrimal glands possess oestrogen and androgen receptor sites, and both hormones can affect the synthesis and components of the tear film.15Lacrimal gland deficiency is seen in women after menopause and after ovariectomy.15 Androgen deficiency is a known risk factor for meibomian gland dysfunction16 –one of the main causes of dry eyes.10
Taking care of dry eyes…
Mild cases of DES can usually be diagnosed in primary care with a trial of first-line treatment and early review.1,17 Patients with symptoms and risk factors for more severe DES need appropriate referral.18
- Early diagnosis and treatment are important to help prevent disease progression2
- DES treatment is related to its symptoms and severity
- Ocular lubricants are first-line therapy for mild DES.2,19
Routine eyelid hygiene may help prevent symptoms particularly if meibomian gland dysfunction or blepharitis is involved.2
… with MURINE® Dry eyes
MURINE® Dry eyes is a specially formulated preservative-free ophthalmic solution that is indicated for dry eyes and offers three benefits for the patient:
- Long lasting dryness relief
- Lubricates dry eyes
- Protects eyes from further moisture loss.
MURINE® Dry eyes contains clinically proven sodium hyaluronate2,19:
- A natural component of the tear film
- Has intrinsic properties of water retention, viscoelasticity, and promotes corneal epithelial wound healing
- Increases viscosity, hydrates and lubricates the ocular surface.
Preservative-free MURINE® Dry eyes comes in an easy-to-use soft-squeeze bottle with a patented filtration system — making it suitable for patients who are:
- Allergic or sensitive to preservatives
- Want to continue wearing contact lenses
- Have problems using hard non-squeeze bottles.
MURINE® Dry eyes can be found in pharmacy retailers at $14.95RRP.