GPs should be comfortable encouraging some people and not others to use doxycycline for STI protection.
As STI rates rise, there’s a lot of interest around doxy PEP in the community, and it was the hot topic at the International Union against Sexually Transmitted Infections (IUSTI) conference in Sydney last month.
The consensus seems to be that it’s an effective intervention for chlamydia and syphilis when specifically targeted, and the message to Australian GPs is that there is guidance on who would benefit, and there is a demand for it too.
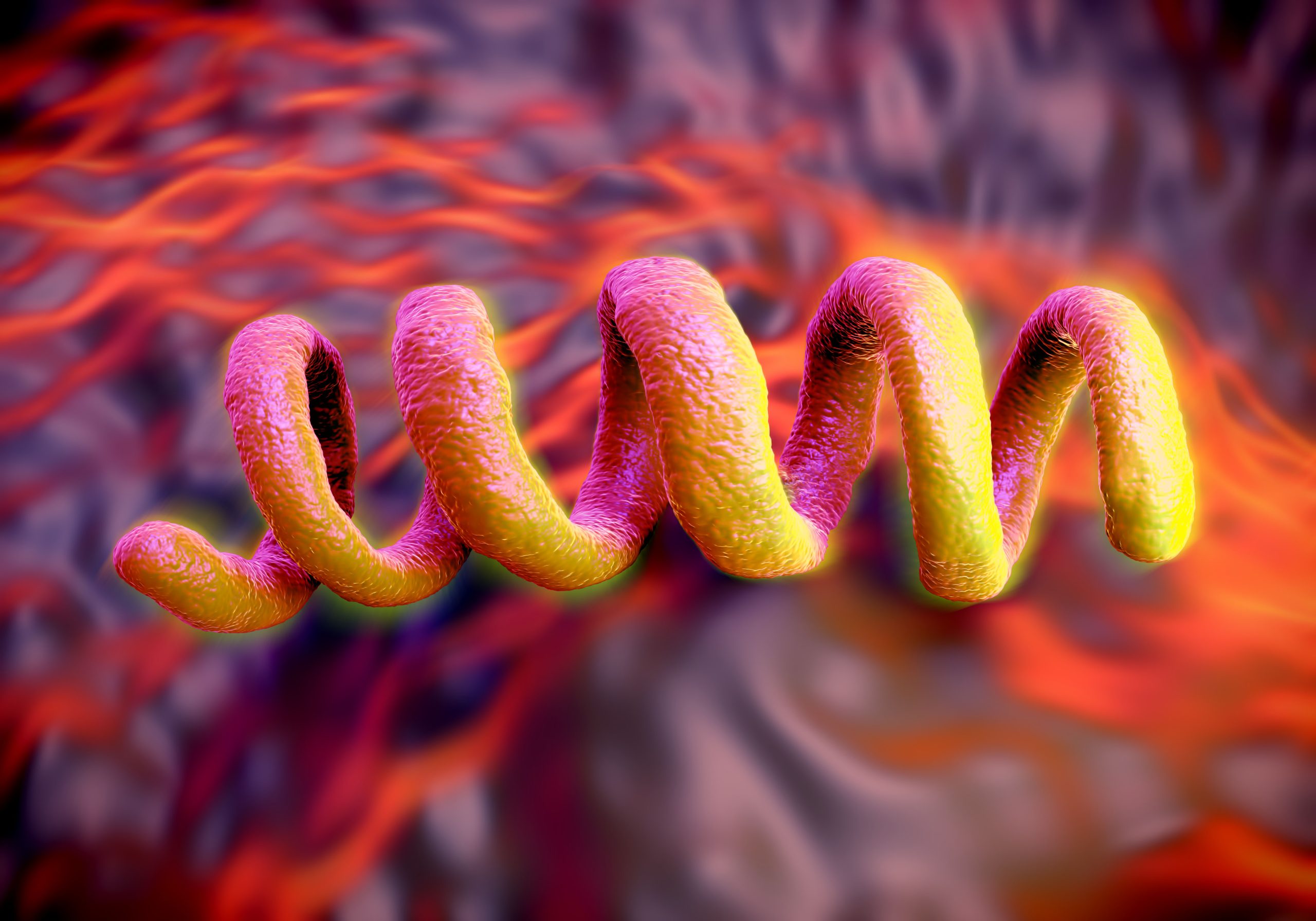
Doxy PEP, or doxycycline post-exposure prophylaxis, involves taking two 100mg pills of doxycycline, ideally within 24 hours but no later than 72 hours after condomless oral, anal or vaginal sex to prevent syphilis, chlamydia and, to a much lesser extent, gonorrhoea.
In randomised control trials, Adjunct Professor Matthew Golden from the University of Washington in Seattle told delegates, doxy PEP has shown a relative risk reduction for all STIs combined of 47-65% and an absolute risk reduction of 32-140 cases per 100 person years. The relative risk reduction for syphilis was 73-89% and absolute risk reduction was 8.6-11.6%.
That meant the typical person took around 43 extra doses of antimicrobials per year to avert 1.4 STIs, comprised of 50% gonorrhoea, 43% chlamydia and 7% syphilis, 70% of which would be asymptomatic, Professor Golden said.
“I think interest in this intervention is very high, and medical providers and public health need to be responsive to that interest while continuing to exercise good medical judgment,” he said.
Syphilis numbers plummet
In Seattle, guidelines have been in place for a year recommending that providers inform specific patients about doxy PEP: MSM and transgender women who have sex with men if they have a history of bacterial STI in the prior year.
The Seattle program has seen a 50% reduction in all stage syphilis among MSM and no change in syphilis rates among women or heterosexual men.
In San Francisco, where the rollout began a year earlier than Seattle in 2023, there was a 51% reduction in syphilis among men who have sex with men (MSM), a 50% reduction in chlamydia in the general population, and no change in gonorrhoea.
“I see doxy PEP as effective at both the individual and population level in preventing syphilis and chlamydia,” Professor Golden said. “It’s our first new intervention that has a meaningful impact on syphilis in gay, bisexual and other men who have sex with men.”
Up to 30% of MSM in Professor Golden’s clinic are on doxy PEP. The regime is integrated into their “demedicalised” PrEP model, where patients see a doctor just once a year unless there’s a problem. More than half of patients who’d had an STI in the previous year were on doxy PEP, and almost 40% of patients who were already on PrEP.
Dr Golden’s Seattle clinic also provides doxy PEP to people who request it, “which is relatively common”, he said.
What about Australia?
In an Australian survey of more than 2000 gay and bisexual men and non-binary people, led by Professor Martin Holt from the Centre for Social Research in Health at UNSW, more than three-quarters said doxy PEP was an acceptable intervention.
“It’s great that there’s such high level acceptability in the community about the strategy, but all the guideline and consensus statements suggest careful targeting and offering of doxy PEP to the people who are most likely to benefit from it,” Professor Holt told TMR. “So we want to hit that sweet spot between offering the strategy to people who may be at higher risk of STIs and hopefully reducing incidence among them, but not giving antibiotics out very broadly to everyone.”
The Australasian Society for HIV Medicine (ASHM) has released a consensus statement which recommends doxy PEP be considered mainly for the prevention of syphilis, but possibly also for chlamydia and gonorrhoea in gay men, bisexual men and men who have sex with men (GBMSM) who are at risk of an STI, ahead of developing guidelines which are due out mid-next year.
“The intention of that consensus statement was to enable people to start doing it if they felt confident enough,” Professor Nicholas Medland from the Kirby Institute, a co-author of the consensus statement and upcoming guideline, told TMR.
“But actually what’s resulted is everybody got a bit confused and is holding back. Meanwhile, syphilis is going skyward, and that’s the health emergency that I think we need to be dealing with.”
Countries and states around the world have their own, differing guidelines, documents, recommendations, position statements, consensus statements and memorandums, and they’re not very clear about when and how to use doxy PEP, Professor Medland told IUSTI delegates.
This is despite them all drawing on the same four RCT trials.
“I think once you put complicated, convoluted language into the guidelines, effectively, what you’re [doing] is giving people permission to talk patients out of it, or you’re putting obstacles in their way, which is a sort of backhanded way of making it difficult for somebody to access something.”
Professor Medland doesn’t think homophobia is behind the hesitancy to clearly recommend doxy PEP in Australia where appropriate, given the people and processes involved in the consensus statement and guideline development.
But “there is definitely something unusual going on with the concerns around this where it just does not happen to be the case in other guideline areas, whether there’s some sort of unconscious sex negative thing, it does seem to come up as a much greater concern than I would have expected,” he said.
Professor Holt said some people involved in the process were “really enthusiastic” about non-barrier method to reduce STIs in the face of rising numbers, others saw doxy PEP as yet another potential avenue for antibiotic overuse, and many were somewhere in the middle.
“Doxycycline is a very reliable and trusted antibiotic and with increasing use in any population, there is a risk of increasing antimicrobial resistance,” Professor Holt said. “And there are other people saying this looks very safe, there isn’t evidence of it increasing resistance in trials, and we could massively reduce, potentially, incidence of syphilis and chlamydia. It’s not going to do much for gonorrhoea, but at least it … might help reduce the massive number of STIs that we’re diagnosing nationally.
“We don’t want to say this is for everyone, because the level of antibiotic use would not be good. But at the same time, we don’t want to dissuade people who’ve had issues with their sexual health from considering it.
“It’s trying to get that non-judgmental, even-handed approach. I think that’s where we’re trying to land, without stigmatising people.”
Not the best target for stewardship
Dr John Saunders, who is leading the development of the UK guidelines, said the issue of antimicrobial stewardship was bigger than doxy PEP and there were better ways to get a bigger impact than “fretting” about doxy PEP.
“Human health is just one element of antimicrobial use, and sexual health is only one small part of human health and antimicrobial use,” he said.
Not implementing doxy PEP was associated with potential harms, said Dr Saunders, citing the upward trajectory of syphilis and the 20 cases of congenital cases of syphilis in Australia last year.
“Levels have never been so high for syphilis since the Second World War … but we have something that might be a bit more effective for some people than a condom.”
Antimicrobial stewardship could be addressed in other aspects of STI care, such as optimising antibiotic use by ensuring testing and treatment were not overdone, he suggested, and creating good guidelines.
“In the absence of a guideline, people will do their own thing. When we surveyed GBMSM to ask if they were using antibiotics to prevent STIs, about one in 10 HIV PrEP users report they are doing this, but about half of those individuals were using something other than doxycycline, so amoxicillin, metronidazole – anything that was left over in the cupboards, really.”
But if the guidelines were to help, they would need to be couched in clear language, he said.
“I think there is a definite risk that the way that some of these guidelines and recommendations can be interpreted as permission to say no to a patient or maybe to spend the time trying to talk your patient out of it. If that’s not what people want in their guideline, then they need to really think about how it’s being expressed.”
In the Seattle experience, tetracycline resistance went from 11-51% between 2021 and 2024, but that trend was well under way before the doxy PEP rollout, said Professor Golden, who blamed the decision to change treatment of chlamydia and N. gonorrhoeae, replacing azithromycin with doxy.
There were also off-target effects of the rollout, said Professor Golden, such as lower rates of group A strep carriage (27% in doxy PEP users vs 36% in non-users), and 66% of the staphylococci found in the doxy PEP users was not resistant to tetracycline, compared to 22% among non-users.
But doxy PEP users had roughly twice the level of group A strep colonisation compared to people who were not on doxy PEP (9% vs 4%), almost all tetracycline resistant.
Practitioners are being urged not to use doxycycline for lower respiratory tract infections or skin and soft tissue infections in people on doxy PEP.
Related
Better from a GP
Because of concerns about judgement, some gay and bisexual men will “compartmentalise” their sexual health and go to someone other than their GP for sexual health matters, said Professor Holt.
“That’s not ideal, because we’d prefer people to get comprehensive care wherever they go, and I think most GPs are fully qualified to do this,” he said. “The research also suggests that GPs, like many other people, are not always that comfortable talking about someone’s sex life. It would so much better for patients and doctors if it was part of routine care.”
In the Australian survey, only 2.6% of respondents were using antibiotics for STI prevention. Just under half of these were prescribed by a doctor, with most of the remainder using leftover medications, getting them from a peer or online without a prescription. Also not ideal.
“Australia, for some reason, is one of the countries where we’re more likely to keep leftover antibiotics and medication,” said Professor Holt. “We don’t want people just randomly using other things optimistically, because we don’t know if it’ll work and it will be, again, a risk of misuse.”
The consensus statement provides examples of the patients who would be appropriate to approach about doxy PEP “and my research suggests that most people will be open to that,” he said.
“In particular, it’s choosing the appropriate moment. If your patients are coming and asking for a sexual health screen, and you’re suggesting one to them, there’s a window there where you could talk about this. Or if they get diagnosed with an STI that would be a perfect time to say, hey, there’s something you could do to prevent this happening in future, if you’re concerned about it.”
There’s a NSW Health online decision tool to help people work out if they would benefit from doxy PEP.
“That’s trying to encourage a conversation: Would this benefit me? Probably a good marker would be if you’ve been diagnosed recently, then probably this is a strategy for you,” Professor Holt said. “But if you haven’t, and you’re testing regularly, then maybe you don’t need this. So, it’s probably for the people who have the busiest sex life. It’s probably the way I’d go at this point.
“If you’re still using condoms or you’re actually getting tested regularly and you haven’t been diagnosed, we probably just want to reassure people it’s not necessary.”