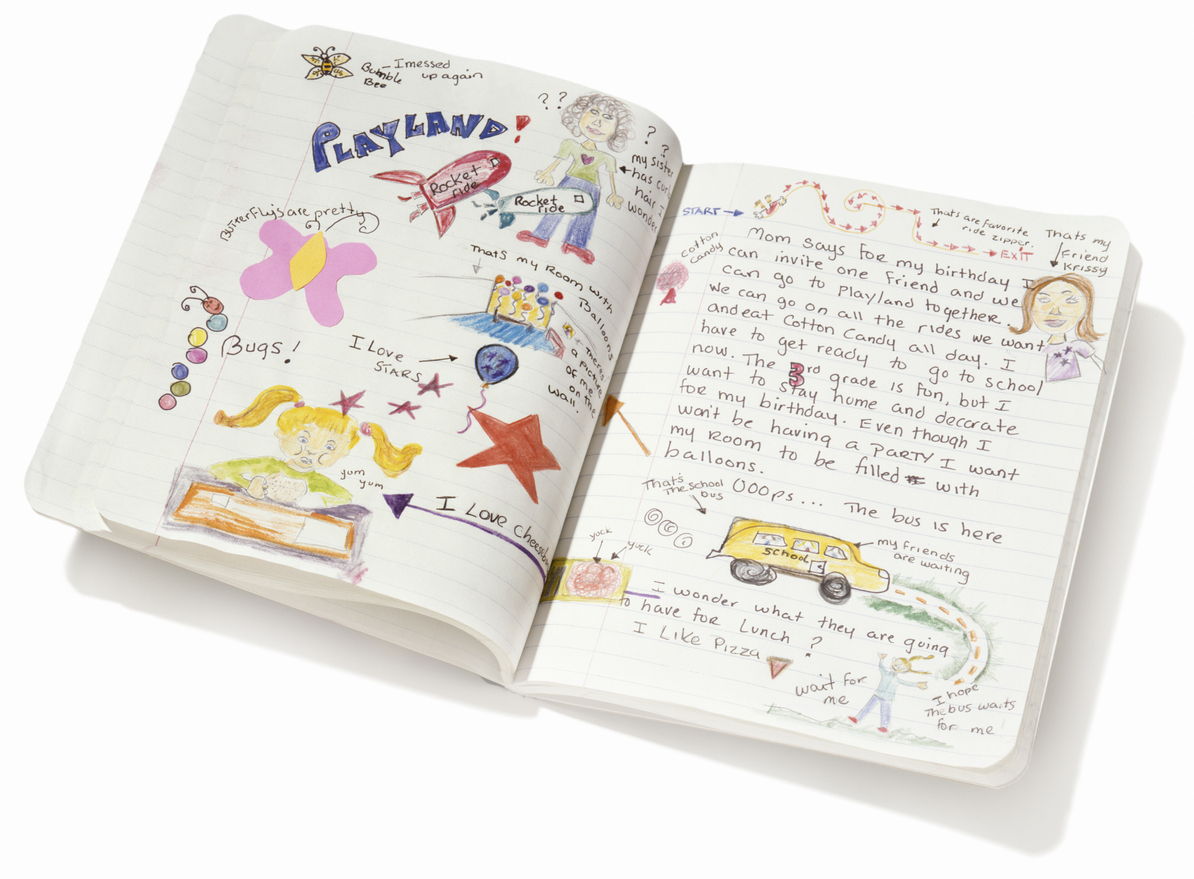
After a rushed but appropriately socially distanced briefing with a government agency policy group this week on COVID-19, someone left their notebook behind
After a rushed but appropriately socially distanced briefing with a government agency policy group this week on COVID-19, someone left their notebook behind
Ever wondered what might be really going on in the minds of our best and brightest advisors to the federal government around the mad goings-on that has been the rapid introduction of full-blown telehealth to general practice over the past few weeks?
A notebook we found following a policy briefing this week (an imaginary one) reveals a fascinating insight from one policy adviser into how the government might actually use the COVID-19 crisis to shepherd general practice into a new era of efficiency that ends up as a win for GPs, the healthcare system, and the government.
Firstly, a bit of context.
The notebook was obviously started prior to COVID-19. It has notes on telehealth initiatives that were started as a result of the bushfire crisis. What seems obvious is that this particular adviser thinks that our current federal health minister is, in fact, a fan of the potential of telehealth.
She notes in the early pages that Minister Hunt seems progressive and motivated, and gets frustrated with the politics of health which creates so little opportunity for meaningful change. He [Hunt] wants to push an innovation agenda to get things done more efficiently and telehealth is on that agenda, but a long term fear exists in the department that telehealth unleashed would blow out the MBS in all sorts of ways and create too many uncontrollable issues.
Our notebook owner observes that the bushfire crisis put telehealth firmly back on the agenda of the policy advisers. It wasn’t a matter of blowouts or unforeseen consequences. It was just a matter of pragmatism in a crisis. Its utility is now obvious far beyond this immediate and practical need in this crisis, says our enigmatic notebook author.
It isn’t long before COVID-19 makes it’s first appearance in the notes. First as snippets of speculation and interest, but soon, as a major focus of all communications going on in the department.
By early March, widespread use of telehealth by all GPs, was an obvious and pragmatic step to take, according to one notation, albeit, with a firm sunset clause in place as there were going to be equally obvious and immediate issues with taking such a step.
Some listed by our author include patient confusion through lack of education, older patients not being able to use the services, GP confusion with boundaries between telehealth and face to face consults, a lack of GP education and training overall, and relatively poor existing infrastructure. Nonetheless, there really wasn’t much alternative given the nature of the unfolding COVID-19 crisis, in particular the requirement for most patients now to be staying at home if at all possible.
What is immediately apparent from our notebook is just how quickly one government adviser comes to understand the real nature of the issues that follow the introduction of widespread telehealth items. Some were apparently quite unexpected by government advisors.
Firstly, the government’s fear of cost blowouts, which caused them to set aside an additional $600 million to meet a predicted frenzy of activity, proves, initially at least, unfounded. A mixture of confusion on the part of GPs who have never used telehealth consults before, a lack of patient awareness and a population now quite fearful of attending their GP in person anyway, created an initial overall drop in total consults, telehealth or otherwise. The government was saving money on the MBS not spending more.
As a result more than half of the country’s GPs have started going broke, with revenues dropping by up to 30% from the same time last year within just a couple of weeks.
Our notebook’s author pens their initial surprise, and footnotes that GPs, though obviously in some shock and distress, are not complaining much, many stating that unlike many of their patients who have just lost their jobs and entire income, they at least have some income and they need to keep going for their patients, and in the context of this crisis, “the system”. They can’t complain … and they don’t much.
That’s a response that begs a few interesting questions on the part of our notebook’s author, for the future of general practice:
- Just how adaptable are these GPs when they need to be? They seem initially to be a lot more adaptable than we have been guessing.
- If we could somehow shepherd them through the darker elements of some of these changes, might they change their ways enough so that on the other side, they are in a better position, and so is the MBS? Could they end up with some sort of structure which efficiently mixes its consult types, and which ends up with all sorts of structural and technological changes which improves their profitability over time, and their working lives? And can we do that while saving the MBS some money?
- Clearly some things will continue to be hard and there will be some casualties of such drastic changes (e.g., some older, smaller practices that can’t or won’t change the way they operate), but with some sort of plan that mitigates the big issues, grandfathers the laggards, and is sensitive to the nature of the sector, can we actually change things for the better here all around?
- Is COVID-19 the once in lifetime opportunity (yes, crisis), for such a step change, which we can’t pass up?
Then our author, does a quick executive summary for us – well, probably not for us, probably for her boss we guess, who we assume could eventually even be Greg Hunt – of where we are. It includes, worryingly, some of the very real and immediate issues that are already starting to emerge which could crash the whole concept in the short term. She notes the government needs to stay on top of the situation day to day even, and iterate to avoid the obvious emerging problems.
Outside of those issues already identified above – infrastructure, training, education, patient education et al – the key emerging issue according to our advisor is the havoc that might reign if tech companies, and, or, large corporate providers of GP services start industrialising the current settings in telehealth and creating a patient population with new and unreasonable expectations.
She notes that it is reasonably obvious already that left to their own devices on the current settings, community general practice networks might rapidly be denuded to the point of becoming entirely ineffective, or indeed financially unviable, in the long term. She notes that this would threaten the viability of key strategic themes for our healthcare system already in place, the main one being that our community GP network is the backbone around which we will be able to longitudinally manage our impending chronic care crisis.
Surprising is that she is well on top of the current the rush by a bevvy of tech companies to either alter their existing telehealth models to an “uber doc” type model, or tangential businesses, such as booking engines, to move upstream into the telehealth game.
She says all are doing what is obvious. Following the money. The MBS money. But less cynically, she observes, some are following the natural need to provide structural support to GPs, in a world where their business model is being structurally sideswiped big time.
She thinks the trend as it is unfolding currently is most unlikely to be healthcare system’s friend. Not when there are virtually no regulatory settings to stop the obvious harvesting of patients who will opt for convenience before anything else when they want an appointment or a prescription. If the harvesting becomes effective quickly, our author estimates that something between 10-30% of low hanging MBS income normally coming through to community general practices will be sucked away to a just a few large groups – some not even healthcare companies.
The Medical Republic concurs with our policy adviser here. At least at this point in time.
Yesterday’s move by major after hours provider National Home Doctor Service (NHDS), to shift their entire model into the provision of 24×7 telehealth services, using their existing after hours workforce and infrastructure, is surely one of the major warning signs of how fast things can change for the government.
A letter sent directly to existing patients of the NHDS yesterday reads:
“We can now also provide you with access to 24/7 telehealth services through our sister business called 24-7MedCare. We have extensive telehealth capabilities that can be offered both via phone and secure video. And don’t worry, if you require a visit by a doctor, we can arrange that as well”
As one GP commented immediately to TMR on seeing this letter:
“Just what we need now. A bulk billed virtual service with no physical presence in direct competition with daytime general practice.”
NHDS is just doing what its private equity owners would demand. Move into a gaping revenue opportunity opened up for them by the new telehealth regime. NHDS has a current business model that isn’t working. Now, they must think they might suddenly have one.
You wouldn’t imagine that our notebook author, on top of things as she seems to be, would be too impressed, especially given how the government moved to close down the after hours providers 18 months ago as the after hour items started to run out of control and cause MBS blowouts. If we’d seen this notebook next week our guess is the NHDS initiative would have a full page dedicated to it with appropriate alarm bells.
As with any major crisis, the opportunities that present themselves to improve things are usually as big as the risks that are presented to destroy things. The NHDS move feels like an obvious loophole that will need to be plugged. Other developments are less easy to judge as to whether they might be good or bad for the healthcare system in the long run.
Take the major appointment engines as an example, and their rapid development and innovation program which is seeing them move upstream, almost into domain of the major patient management systems. It is going to be almost impossible to tell if what they are doing now to adapt to telehealth is going to ultimately lead to improvements or issues in the system.
HealthEngine is not quite there with it’s fully integrated telehealth solution yet, but it is likely to get there soon. So is HotDoc.
HealthEngine founder, Dr Marcus Tan, has always maintained that HealthEngine is a healthcare company before it is a tech company and that he has always tried to build systems that assist the community general practice network. In practice so far, apart from the company’s data privacy event, this seems arguable. An internet directory network and widely downloaded patient app, that means your practice and key criteria around your servicing capability is accessible to patients 24×7, and an increasingly functional and seamless telehealth solution for any practice that wants to adopt it.
But looked at another way, HealthEngine might be building a platform which might end up creating the same issues for doctors, that hotels and other travel service providers now face with the major global booking platforms such as Booking.com.
A patient wants an appointment for a particular type of consult. HealthEngine polls the patient’s normal GP but they either don’t have one available immediately (convenience is now in play remember) or they don’t have the right have facilities for the consultation the patient is after. The enquiry is hence re-directed to the next closest geo-located practice to try to keep the consult at least in the local community. But that doesn’t work either, so the system defaults to most available. Most available turns out to be an industrialised provider – maybe even NHDS. If industrialisation of telehealth is allowed, it seems obvious that ‘most available’ will be dominated by a tech or corporate service not a community GP.
You can see how easily such a system might end up where even Dr Tan might not even be contemplating. You can see that our notebook author has a big job ahead keeping on top of such rapid evolution in a system that until now has not changed itself for decades meaningfully. You can see why Dr Harry Nespolon, who is in the corner of community GPs fighting day and night, still admits that the telehealth regime introduced has only managed to bring GPs up to the year 2007, the year the iPhone was introduced.
HotDoc and HealthEngine are becoming increasingly influential and powerful. Being cloud based platforms makes them highly agile in development and delivery. They are moving upstream into the realm of the patient management vendors who can’t be as agile because they these are complex systems still running on old technology where integration with other systems is more difficult. The booking engines also are attempting to bring power to the patient in the healthcare equation. Although the patient management systems control access to the GPs, the booking engines control the consumer. This battle and how it balances it out over time, and who ultimately controls what, is an important factor in how health care might end up being delivered. Remember, Best Practice has a patient app themselves now, and in theory, that means BP might end up with direct access with up to 12 million patients.
As the after hours services failure has shown, patient convenience does not win out over cost of system delivery. Healthcare isn’t as simple as banking or travel in this respect.
Back to our notebook and its author.
In a worst case scenario tech companies, corporates (including the after hours providers), act so quickly and adroitly here that the public rapidly adopts a new paradigm, in which community GPs are reduced to doing only the most complex and expensive face to face work. Some precedence exists for this in the rise of the Babylon health service in the UK, something which is causing havoc for NHS primary care services.
What if GPs become reliant on consumer driven platforms to survive, just as the hotels and travel services worldwide are now all not able to do business without the consumer facing distribution platforms – Expedia, Bookings.com, AirBnB – all of which charge the service providers exorbitant access fees?
Our notebook author can’t even imagine what all this might do the MBS and overall costs of primary care. She simply scribbles ‘MBS effect…’ followed by multiple question and exclamation marks.
But she is optimistic. She notes that the learnings from both the bushfire and COVID-19 experience are coming at them fast and the most important thing for her and her colleagues is too keep an open mind on the opportunities and do their best to understand and moderate the potential risks. She is adamant that the government ‘should not waste the crisis’. The opportunities, in her mind, are outweighing the risks.
The last few pages of the notebook have been ripped out, but there are some notes scribbled on the cardboard inside back cover that probably speak for themselves.
Why is industry jumping in with so much investment and vigour when everyone knows there is a sunset on all these telehealth items in September?
Do they think (realise?) that we can’t ever put this genie back in the bottle now?
What happens if we do just put the stop back on the bottle? That might be more damaging in the in short and long term given what is going on!
What do we do now?
I don’t think we can waste what we’ve learnt, and I doubt patients and doctors will want us to either.
We let this genie out so if this is ends up a success or a mess is really down to us. This is much bigger than anyone thought. Upside and downside.
We need to work fast and smart here!
The (imaginary) notes end there.
But we like to think that given a bit more space she might have written – then we can all go back to sleep again.
As per every Saturday now, other good stories from the week follow. See you next week.