Summer is on its way! And along with the heat comes the potential for dehydration and heat-related illnesses.
Summer is on its way! And along with the heat comes the potential for dehydration and heat-related illnesses.
Preventing and treating these ‘symptoms of summer’ is important and choosing the appropriate oral rehydration solution (ORS) is an easy first step in managing mild to moderate dehydration.1-3
Hydralyte®, formulated to meet World Health Organization (WHO) ORS recommendations, has the correct balance of water, glucose and electrolytes for rapid rehydration and restoring electrolyte balance.1,4
The challenge with summer
Summer in Australia can pack a punch, with heatwaves, water restrictions and bush fires becoming a regular feature with more Australians likely to be feeling its negative health effects.5
Dehydration and heat-related illnesses (plus other unrelated illnesses affected by heat) can be a particular challenge during the summer months. Australian summers are getting hotter with the country recording its hottest day on record in December 2019 (peaking at an average of 41.88°C) and the number of heatwave days increasing across the major cities — meaning large numbers of Australians are increasingly having to endure dangerous heat conditions.6
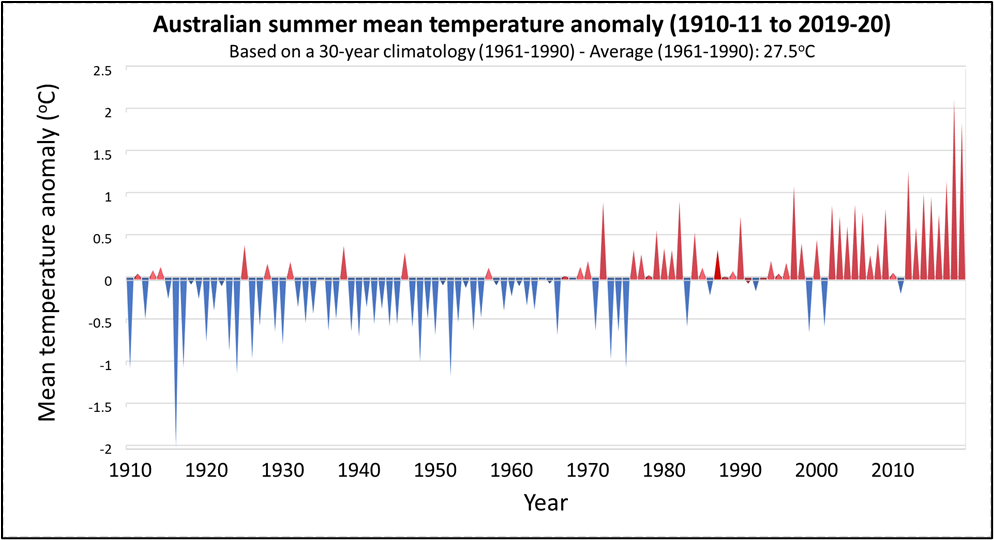
Source: Australian Beureau of Meterology (http://www.bom.gov.au/climate/change/) CC BY 3.0 AU
The challenge with heat
When exposed to warm or hot ambient temperatures for prolonged periods the human body starts to warm up. This ‘heat accumulation’ is related to the combined effects of environmental exposure (e.g. temperature, air-movement, shade), metabolic demands being put on the body (e.g. exercising or resting) and whether the body’s cooling mechanisms are restricted or impaired in some way.7
The hypothalamus, the body’s internal ‘thermostat’, helps facilitate heat loss and maintain a normal core temperature primarily by increasing sweat production, but also by increasing cardiac output and diverting more blood to the peripheral vessels in the skin.7
Most healthy individuals are able to regulate body temperature through the skin via a range of cooling mechanisms:8,9
- Evaporation — the most effective method of excess heat dissipation to the surrounding air (via sweat or other liquids on the skin’s surface)
- Radiation — which does not require air-movement or direct contact with skin
- Convection — transfers heat to either a gas (the air) or a liquid moving over the body; this also helps improve heat loss by evaporation
- Conduction — transfer of heat to a cooler object by direct skin contact.
As the ambient temperature rises people can start to feel irritable and their ability to carry out skilled tasks or heavy work can be affected — temperatures above 30°C can impact on the performance of mental tasks and manual labour (and sport) can add to the body’s heat burden.10
Dehydration (a major risk factor for heat-related illnesses) develops if fluids lost, for example through sweating, are not replaced.7 Intense exercise or work activity in heat with excessive sweating can make things worse causing a decrease plasma circulating volume and hypovolaemia affecting the body’s ability to cool7 — studies suggest that for every 1% body mass lost through dehydration there may be an increase of 0.21oC in the core body temperature.8 Early detection and treatment of dehydration is important as it can progress rapidly if oral rehydration is not addressed — with mild symptoms quickly worsening. 3,11
Early signs of mild dehydration for patients to watch out for include:11
- Thirst
- Dry mouth
- Headaches
- Reduced concentration
- Darker (more concentred) urine.
Problems start to arise when heat accumulation exceeds the rate of heat loss and the homoeostatic mechanisms in the body are overwhelmed increasing the risk of heat-related illness occurring.7 Symptoms vary according to the type of heat-related illness:
- Mild heat-related illnesses — conditions that are usually self-limiting such as heat oedema (typically in the lower limbs), muscle-cramps and heat rash (miliaria rubra).7
- Moderate heat-related illnesses — conditions such as exercise related collapse (symptoms include light-headedness, orthostasis, dizziness, transient loss of consciousness) and heat exhaustion (symptoms include thirst, headache, fatigue, tachycardia, weakness, ataxia, syncope, nausea, vomiting, diarrhoea and a core temperature of 38.3° to 40°C)7
- Severe heat-related illnesses — such as exertional heatstroke (symptoms include altered mental status, seizures, coma, tachycardia, hypotension, hyperventilation, diaphoresis and a core temperature ? 40.5°C).7
Major risk factors for heat-related illness include:7,12
-
Exposure to high ambient temperatures (above 37.8oC)
-
High humidity
-
An increase in body heat (via increased metabolism or muscular exercise)
-
Over-insulation (such as wearing protective gear or excessive clothing)
-
Alcohol consumption and certain medications (such as diuretics and beta-blockers)
-
Lack of acclimatisation
-
Dehydration through lack of fluid intake or excessive sweating.
Vulnerable groups
Although everyone is at risk of dehydration and heat-related illnesses during hot weather some people are more vulnerable than others. For example, those with compromised heat regulation processes due to their age, medications, illnesses or other conditions, or who work or train outdoors.7
Pregnancy
- Many women tend to feel warmer during pregnancy. Their basal metabolic rate (and thus heat production) tends to be above their non-pregnant levels making them potentially more susceptible to dehydration – particularly under warm or hot environmental conditions.13
- Guidelines recommend regular aerobic and strength conditioning exercise for their overall health benefits during uncomplicated pregnancies — but patients also need to be advised not to overheat during exercise due to the potential for foetal harm.14,15 Although data on the effects of pregnancy exercise and core temperature are limited, foetal core temperatures are around 1oC higher than the mother’s.13
- Braxton Hicks contractions may be triggered under certain conditions including dehydration and may be linked to the need for increased blood flow to the placenta.16
- Pregnancy may trigger feelings of nausea, poor appetite and vomiting which can add to the potential for dehydration under hot conditions.17
Babies and children
- Young children and babies are at greater risk of becoming dehydrated than adults having higher water requirements per unit of body weight – the water is also distributed differently with higher levels in the extracellular than intracellular 18
- The risk of developing heat-related illness is also increased as they are not able to adjust to environmental changes in temperature as well as adults do – for example, they sweat less (reducing heat dissipation) and produce more heat while exercising compared to adults.19
- They are also potentially more likely to be spending time outdoors engaged in physical activities and may be dependent on adults for access to fluids.
Older adults
- Older adults are at increased risk of dehydration and heat-related illnesses (including non-exertional heat stroke) and may need special care in hot weather7
- Hydration levels may already be depleted due to a reduced thirst reflex and renal dysfunction3
- Chronic conditions or confused states may exacerbate or increase the risk of dehydration3
- They are more likely to be taking medications — some of which may increase the risk of dehydration e.g. duiretics3
- Limited mobility or the dependence on others may hinder access to fluids3
- Lack of air-conditioning or other means of cooling may compound heat-related problems.7
Treating dehydration
Knowing how to recognise the signs of dehydration and other heat-related illnesses is important for vulnerable patients.9 Providing patient education on how to behave during extreme conditions, what warning signs to look out for and when to seek medical help is an important role for the primary healthcare giver.9 Advice on fluid and electrolyte intake during times of extreme heat conditions, prolonged exertion or high humidity should also be discussed.9
Replacing lost fluids and electrolytes is the most important initial step in managing dehydration – a major risk factor for heat-related illnesses.7 Oral rehydration solutions — such as Hydralyte — are appropriate for adults and children with mild to moderate dehydration, supplying maintenance requirements by correcting volume and electrolyte deficits and replacing any ongoing abnormal losses.1
Why Hydralyte
Hydralyte is specifically formulated to meet WHO ORS criteria for effective hydration — helping to replace water and electrolytes lost due to heavy sweating, vigorous exercise and other dehydrating conditions encountered during the Australian summer:4
- Electrolyte Ice blocks: cools and hydrates — ideal for hot weather hydration
- Oral Electrolyte Solutions: ready-to-use when needed
- Oral Electrolyte Powder: compact and portable for travel and on the go
- Oral Electrolyte Effervescent Tablets: convenient on the go solution
The Hydralyte range:
- Suitable for all ages (0 – Adult) and life stages including during pregnancy and breastfeeding
- Have the correct balance of sodium and glucose in-line with WHO ORS recommendations
- Are hypotonic — allowing effective rehydration while minimising potential side effects such as a feeling of fullness/bloating
- Have a lower sodium content – formulated specifically for the diets of developed countries
- Contain low sugar
- Available in a variety of formats and flavours.
For further information contact Care Pharmaceuticals: FREECALL Australia 1800 788 870 www.hydralyte.com.au
References
- World Health Organization (WHO). Oral rehydration salts. Production of the new ORS. 2006. Available at: https://www.who.int/maternal_child_adolescent/documents/fch_cah_06_1/en/ (accessed September 2020).
- Harris C, et al. Aust Fam Physician. 2008;37(6 Spec No):22?29.
- Woodward M. Guidelines to effective hydration in aged care facilities. Aged & Residential Care Services, Heidelberg Repatriation Hospital. April 2013. Available at: https://www.semanticscholar.org (accessed September 2020).
- TGA Public summary. Hydralyte Orange Flavoured Electrolyte Powder. Available at: https://www.ebs.tga.gov.au (accessed October 2020).
- Steffen W, et al. Summer: Escalating Bushfire, Heat and Drought Risk. Climate Council of Australia. 2019. Available at: https://www.climatecouncil.org.au (accessed October 2020).
- Australian Bureau of Meteorology. Special Climate Statement 73—extreme heat and fire weather in December 2019 and January 2020. 17 March 2020.
- Gauer R, Meyers, BK. Am Fam Physician. 2019;99(8):483-9.
- Pryor RR, et al. Wilderness Environ Med. 2015;26(4 Suppl):S69-75.
- Sankoff J. Aust Fam Physician. 2015;44(1-2):22-6.
- CCOHS. Hot Environments – Health Effects and First Aid [Online]. Last updated August 2016. Available at: https://www.ccohs.ca/oshanswers/phys_agents/heat_health.html (accessed October 2020).
- Campbell, N. Nursing Times. 2014;110:20-1.
- Del Bene VE. Temperature. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 218.
- Artal R, O’Toole M. Br J Sports Med. 2003;37(1):6-12.
- Brearley AL, et al. J Physiother. 2015;61(4):199-203.
- RANZCOG. Exercise during pregnancy. C-Obs 62 [Online]. Last reviewed March 2020. Available at: https://ranzcog.edu.au/ (accessed October 2020).
- Raines DA, Cooper DB. Braxton Hick contractions [Online]. StatPearls. Last Update 11 August 2020. Available at: https://www.ncbi.nlm.nih.gov/books/NBK470546/ (accessed October 2020).
- Patil CL, et al. Ecol Food Nutr. 2012;51(5):394?417.
- EFSA Panel on Dietetic Products, Nutrition, and Allergies (NDA); Scientific Opinion on Dietary reference values for water. EFSA Journal 2010; 8(3):1459. [48 pp.]. Available at: www.efsa.europa.eu (accessed October 2020).
- NSW Heath. Babies and children in hot weather [Online]. Last updated 19 December 2019. Available at: https://www.health.nsw.gov.au/environment/beattheheat/Pages/babies-children-hot-weather.aspx (accessed October 2020).


