Is general practice leadership making good progress in bringing government and other key external stakeholders over to their side, or do we have a bigger problem that we might be missing?
There was a point near the end of Burning GP last weekend where I think I could have easily ruined most of the good work of the whole conference (it’s going to be on video soon and some of it was great), indeed, perhaps ruined The Medical Republic business.
We were near the end of what I thought was a really good meeting. Like The Medical Republic and its sister brands Wild Health and now Health Services Daily like to do, we had attempted to get the right people into the room and talk about stuff that was normally off limits for being too controversial or complex to air publicly or simply too touchy to get across to a more diverse crowd.
But we did a lot of preparation with speakers and panellists to orchestrate a pretty tricky middle ground where you don’t burn anyone speaking or anyone in the audience, but you manage to get issues on the table that don’t usually make it to the table in a largish gathering of GPs, government, technology vendors and other important stakeholders.
These topics require a reasonable amount of self-reflection about why we are where we are. Not everyone likes self-reflection. And most people don’t like change.
Anyway, it’s pretty exhausting do an event like this and I was getting very tired, and right near the end, a well-meaning and frustrated GP got up and went on a pretty big rant about what was wrong with the world and what they would and would not do about it.
It was in many respects an understandable rant. It was one that came from a place of what I’m going to guess was quite a bit of isolation from the real (and at times bizarre) world of Canberra, state politics, the huge emerging technology changes in play, and the feeling of being trapped within so many aspects of at times wicked changes.
Anyway, I was on the job taking around microphones to the audience for questions, and, forgetting I had a live mic in my hand, I turned to one of our staff and said stuff that if the live mic had tripped into “on” (it was thankfully just out of range I guess), I may have been ritually taken outside and strung up in the nearest palm tree by some in the GPs in crowd.
I’m not going to go into the gory detail but I started with: “… and there’s the bloody problem right there …” The rest was pretty bad on my part given what the conference was trying to do: get the core issues out on the table for a lot more to see and think about without judgement, fear or favour.
I was being pretty judgemental.
That GP was clearly struggling to get on top of some of the issues at hand and was super frustrated. And I’m going to guess they had every right to be.
It was a pretty good illustration for me of what I had attempted to pitch to this tough crowd the day before: a lot of the problems of general practice have a single root cause that I think that GP leadership is either missing, or, if they get it, they aren’t getting out front of.
Culture. Specifically, the culture of medicine, GPs and politics.
I know that although there was nothing wrong with what that GP got up and ranted about near the end, there were very influential stakeholders in the room, who rolled their eyes like me, thought a lot worse than me of it ( I have reflected and confessed here after all, at least a bit above), and pocketed their thoughts quietly in the back of their brains somewhere that imbedded even more bias against general practice that is neither a correct bias or fair.
But whose fault is it that some stakeholders in that audience went this way?
I don’t think you can blame the frustrated ranting GP.
But GP leadership in general might need to think a bit harder on why that GP got up and said what they did, and what effect it almost certainly had on some influential non-GPs in the audience.
In my talk on the topic the day before I tiptoed into the idea that there are a lot of key people in government, many of them running GP policy or at least importantly tangential to it, that actually don’t like GPs.
The point was part of a set of cultural themes that I presented for everyone to consider about how key stakeholders have seen GPs in the past, and how, although many of these themes were now clearly out of date, many key stakeholders had not got the memo on that. Each formed a part of how some stakeholders frame how they thought about GPs and general practice.
The slide in question is below:
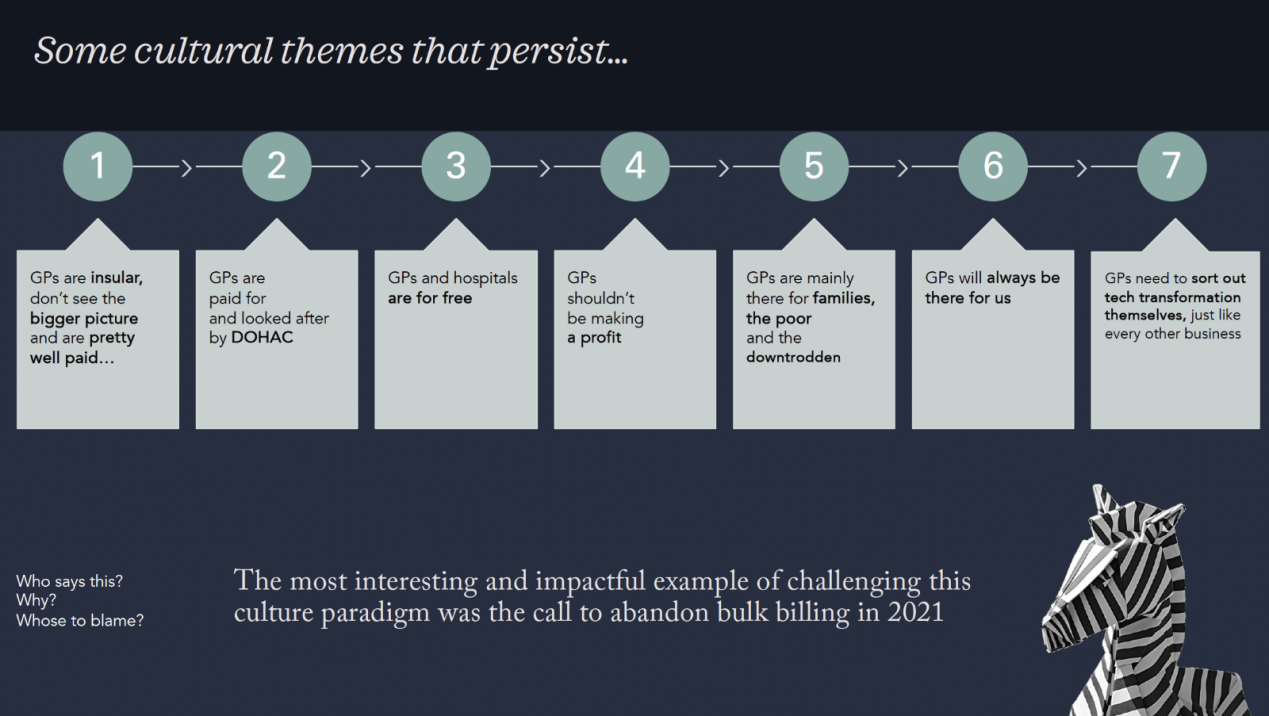
Some cultural themes that persist about GPs include:
- GPs are insular, don’t see the bigger picture and are pretty well paid.
- GPs are paid for and looked after by the Department of Health and Aged Care.
- GPs and hospitals are for free.
- GPs shouldn’t be making a profit.
- GPs are mainly there for families, the poor and the downtrodden.
- GPs will always be there for us.
- GPs need to sort out tech transformation themselves, just like every other business.
The first of these themes – that GPs are insular, don’t see the bigger picture and are pretty well paid – you might recognise. It was the key one I put up to demonstrate what I often feel the vibe is when talking to key people in state and federal politics, and worse, in departments of health (state and federal).
I happen to know most of the department of health people in the room at Burning GP and they haven’t bought into that theme at all, which should be good news for GPs.
But when that GP got up and ranted, some people in the room would have done what I did, and blamed that GP (I have recanted remember).
But a question I put to the room – too timidly I suspect – was, who is to blame for this cultural theme persisting in government and among key stakeholders in policy?
Because it isn’t the people in the departments who retain this bias against general practice.
Let’s not blame the GP who got up frustrated either.
GP leadership has to get in front of this very real problem of cultural overhang about GPs and what they should or shouldn’t be doing and how they should be behaving, and work on changing these cultural overhands.
There are some doing it, but I suspect they need to do it much better, much quicker.
In case you hadn’t realised, all of the cultural themes above, which may have once been relevant in some way, are not what is real these days.
The problem is, a lot of influential people still use these themes to frame how they view general practice.
That’s how culture works.
In case I’m depressing you, here was my next slide (don’t worry about the Zebra):
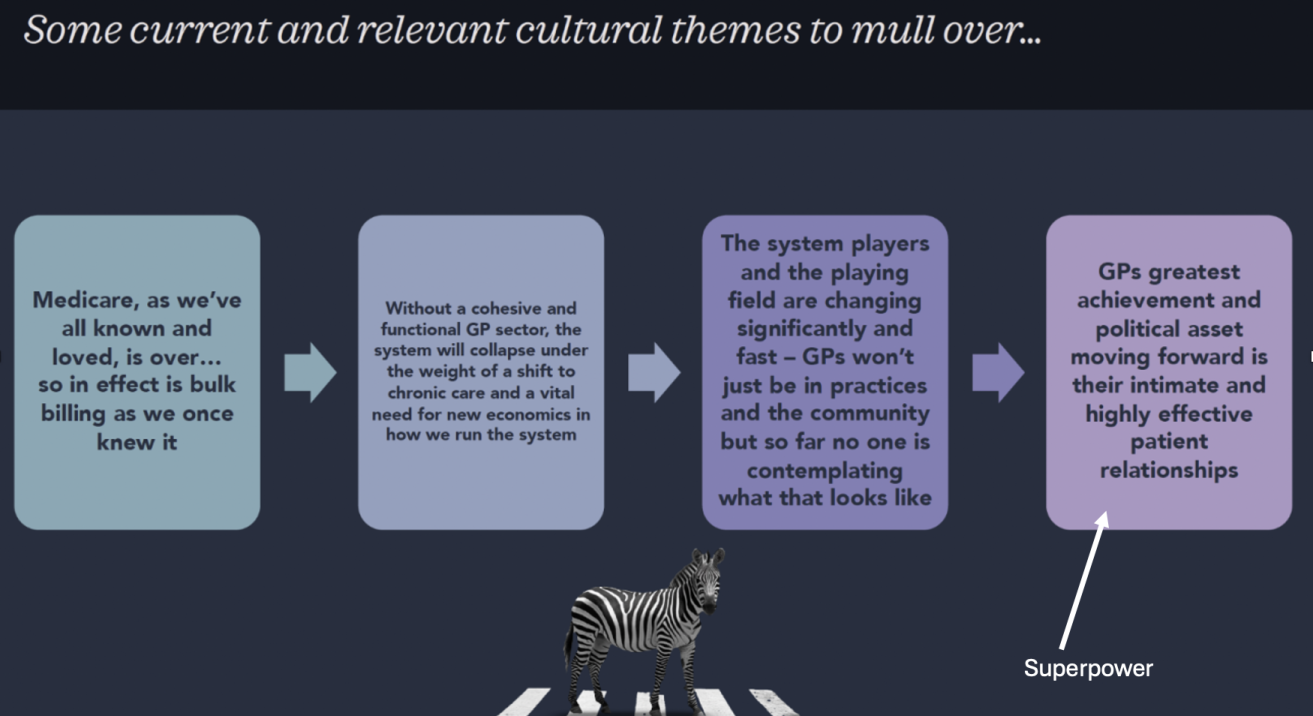
- Medicare as we’ve all known and loved it, is over…so in effect is bulk billing as we once knew it.
- Without a cohesive and functional GP sector, the system will collapse under the weight of a shift to chronic care and a vital need for new economics in how we run the system.
- The system players and playing field are changing significantly and fast – GPs won’t just in practices and the community but so far no one is contemplating what that looks like.
- GPs greatest achievement and political asset moving forward is their intimate and highly effective patient relationships.
These themes, in my view (let’s face it I’m an outsider looking in and making some observations), are much more representative of what is real, and how someone should be thinking if they want to put GPs through some sort of relevant cultural filter.
The trick here is to get us all from that first slide to the second in the minds of the stakeholders that matter.
That, in my old world as a CEO of a pretty big corporate sitting within a giant global corporate, is what we might have all called strategy framing.
Looking at it another way, instead of being reactive and defensive on a lot of the problems facing general practice, which GP leadership tends to be (not all for sure so don’t get defensive straight away), look at all these problems first through the filter of what I am suggesting might be a key problem: culture.
A quick example of what I’m trying to get at here.
This week, NSW came out and promised to create legislation which would not levy payroll tax on any general practice that did 80% or more of bulk billing.
Strangely, local RACGP leadership came out and said they supported the initiative and said it was a good thing.
But if you look at the socials and talk to key people behind the scenes, most GP leadership sees the NSW initiative for what it is: ignorance, coercion and a complete lack of understanding of the plight of GPs and how monumentally ineffective such a policy would actually be at reducing the burden on hospital EDs in the state.
But it wasn’t only the NSW government missing the point entirely.
The media missed it as well. It was described by various large media organisations as a major policy that was a win for GPs and a win for hospitals because it would address the ED problem.
What is wrong with this picture?
Quite a bit, and you could put a lot of what happened down to the first negative culture slide above. State politicians do not understand the GP problem, they are focussed entirely on their ED problem, so they figure that a little bit of blackmail won’t hurt.
They don’t pay GPs and they aren’t paying any attention to the real plight of GPs financially (they think they are well paid and whingers remember) so they think that such a policy is great all around. They might even think that the policy is good for GPs but the logic on that is pretty warped because it would be, “we won’t ruin you with payroll tax, which we have never collected in the past anyway, if you just be good and bulk bill a lot more, and in doing so, go broke eventually…thanks”.
The other thing wrong is that the NSW RACGP came out and said they welcomed the policy.
We know the NSW RACGP was working their rear ends off behind the scenes for something a lot different to this, and educate the NSW government about the real problems.
But they failed. They probably failed because the cultural frame in which state politicians view general practice needs so much work.
But why come out and say you welcome such an obviously damaging and stupid policy?
I’m going to say it’s culture again. Which is to say, payroll tax isn’t actually the big problem…how state governments frame how they see GPs is. If they saw them in the right frame, possibly no state government or politician would have ever embarked on such a crazy political and system destabilising journey with respect to the tax.
Culture is a tricky beast. It’s imbedded deep in each of our psyches. Racism is a pretty gory cultural issue for Australia, to give you some idea of just how hard it is to try to manipulate and change culture.
Anyway, I’m just ranting and spit balling here (as ever), but I’ve left the best bit (and slide) until last.
It’s a sort of cultural end game for the next 10 years if you will and I really think it’s feasible because GPs have a superpower they’ve not even begun to unleash on those pesky politicians, policy makers, tangential healthcare professions and even the tech vendors who make their software.
That superpower is the last point in the slide before this one but if harnessed it can easily lead to this slide.
GPs’ superpower of course is their intimate, longitudinal and highly effective relationship with their patients.
The cultural frame here is interesting. A lot of patients love to trash GPs for being uppity and rich and aloof and all knowing. But patients rarely trash their own GP (there’s a talk in Burning GP on it which we will put up in a week or so). In fact they tend to love them and rely on them a lot. A lot of patients will put down general practice broadly but stick up for their GP as if their GP a special outlier.
What most of those patients don’t realise is that their GP isn’t that special. Most patients think their GP is special, which technically should mean all patients are behind general practice.
But they aren’t as a whole.
Yet.
It’s an interesting problem and GP leadership needs to get in front of it…patients individually love their GPs, but are prepared to accept cultural framing about the profession generally which is quite different.
A fascinating way one GP leader cut this problem up a few years back was to come out as the president of the RACGP and tell every GP that the gig was up and they needed to start mixed billing any patient they thought could afford it.
Adjunct Professor Karen Price maintains that she didn’t seek any permission from the RACGP board to do this. That it was born of deep frustration and desperation and she didn’t give it a ton of thought before she did it.
Whatever it was, it stands as the single most important initiative in the history of general practice in terms of crashing through outdated cultural norms that hold back general practice.
If you go back to the slide on persisting cultural themes that are now wrong but still framing how people deal with general practice, the call to arms to effectively abandon bulk billing has done more to kill off that list than anything else GP leadership has done before or after.
And the most fascinating thing about it is, the patients didn’t blame the GPs for having to pay. They largely have started blaming the politicians.
Patients do like their GPs on mass it turns out, and they are starting to understand a lot better the dilemma that GPs are facing. Having to pay for their consult made them think a lot more about what is going on.
Turns out, some didn’t care about paying, and others who did, still pay anyway because they sort of get it.
Of course, there are big problems still on the many patients who are falling through the cracks.
But if you think that through there is a huge cultural theme at play here too.
GPs didn’t become GPs to make money like pharmacists generally do (this explains why GP leadership can never copy the success of the Pharmacy Guild in lobbying). They became GPs do help patients and do good medicine. So asking patients to pay was a huge moral dilemma for many GPs.
But GPs are small businesses too. And most were on a path to going broke.
Asking patients to pay – even asking the only ones that can pay to pay – has been a huge personal dilemma for a lot of GPs none the less.
But do the public think GPs are free anymore?
GPs were never free. But everyone, including a lot of state politicians really did think that GPs were a free government service. And if they aren’t they should be – hence why the NSW, Victorian and SA governments all think its fine to try to force GPs back into bulk billing, even though that is going to send them broke and destroy the system.
It’s been hard, but that cultural overhang is one its way out at least.
And probably just in time too.
Possibly without realising it, the call to abandon bulk billing became the first really interesting and powerful strategy that GP leadership put in place to start properly getting in front of this cultural problem GPs have.
In one session at Burning GP I very nearly got booed off stage for saying GPs don’t like change (it’s pretty universal that every person and profession hate change but hey I gave it a whirl).
I insulted quite a few GPs in the room clearly. Some even stood up and said they embrace change as a part of their everyday practice of medicine.
Which I’m pretty sure they do.
But that’s not the sort of change I was talking about.