A comparison of excess all-cause mortality in New York City during the 1918 Spanish flu and during the COVID-19 pandemic has found that the Spanish flu epidemic was associated with 30% lower excess mortality.
Welcome to The Medical Republic‘s COVID Catch-Up.
It’s the day’s COVID-19 news into one convenient post. Email bianca@biancanogrady.com with any tips, comments or feedback.
13 August
- COVID-19 shows higher excess mortality than the 1918 Spanish flu.
- Most secondary infections occur in household contacts, study finds.
- Second COVID-19 surge in Texas in younger, lower-income and healthier individuals.
- Editor of Science cautions against dangerous rush for COVID-19 vaccine.
- Non-invasive ventilation can be considered for COVID in negative pressure rooms.
- Children account for 1% of COVID-19 cases in the UK.
- Public health warning as three staff at Sydney’s Liverpool Hospital test positive.
- Latest confirmed COVID-19 infection numbers around Australia.
- Take a bow, SARS-CoV-2: you’ve beaten the Spanish flu for excess mortality. A comparison of excess all-cause mortality in New York City during the 1918 Spanish flu and during the COVID-19 pandemic has found that the Spanish flu epidemic was associated with 30% lower excess mortality.
1918 was hardly a high point for public health, and came at the tail end of a world war that would have left a huge number of otherwise healthy individuals in a damaged and battered state. So the fact that COVID-19 has still claimed more lives suggests it really is the nasty of nasties, at least of the respiratory variety.
The study, published in JAMA Network Open, found that the peak of the 1918 H1N1 was associated with a 2.8-fold higher rate of all-cause mortality compared to corresponding periods from 1914-1917. The peak of the COVID-19 pandemic is associated with a greater than four-fold higher rate of all-cause mortality than the same period from 2017-2019.
“We believe that our findings may help officials and the public contextualise the unusual magnitude of the COVID-19 pandemic, leading to more prudent policies that may help to decrease transmission by decreasing the effective reproduction number of SARS-CoV-2 and prevent the exhaustion of essential supplies of life-saving resources in the coming weeks and beyond,” the authors wrote. How delightfully optimistic.
(P.S The headline for this was nearly ‘COVID-19 beats Spanish fly’, which led to much snort-laughing before it was corrected [Spanish fly is an aphrodisiac of dubious efficacy] and goes to show that Friday afternoon is a very risky time for typos). - Among all close contacts of COVID-19-infected individuals, those they share a household with are most likely to be secondary infections, research suggests.
A study published in the Annals of Internal Medicine analysed data from 3410 close contacts of 391 index cases of COVID-19, and found 127 (3.7%) were secondarily infected. More than 82% of the secondary infections were household contacts, with around 5% from healthcare settings, 8% in workplaces or entertainment settings, and less than 1% from public transport. The overall secondary attack rate among households was just over 10%, similar to what has been seen in other studies.
The more severe the index case, the greater the rate of secondary infections. When the index case was asymptomatic, the secondary attack rate was just o.3%, compared to 6.2% for severe or critical cases. - A comparison of patient demographics in the first and second COVID-19 surges in Texas has found patients in the second wave tend to be younger, with lower incomes, lower comorbidity burden, and more likely to be Hispanic.
Writing in JAMA, researchers reported the outcomes of an electronic health record study of 774 patients hospitalised with COVID-19 during the first surge, and 2130 patients hospitalised during the second surge.
The study found that fewer patients in the second surge were admitted to intensive care and their length of hospital stay was shorter. During the second surge, in-hospital mortality was also significantly lower compared to the first, except among those admitted to intensive care where there was no significant difference.
“The demographic and socioeconomic shift may reflect return to work and relaxation of COVID-19 transmission mitigation practices,” the authors wrote. - Science magazine editor H. Holden Thorp has warned against the ‘dangerous rush’ to get a COVID-19 vaccine to market.
In an editorial, Thorp pointed out that the race of “Sputnik” proportions was being driven by political goals, but short cuts in testing of vaccine candidates could endanger millions of lives and damage public confidence in vaccines.
“In the United States, the pressure applied to government scientists by the administration on any aspect of the pandemic is becoming increasingly palpable, as they have been criticized or quieted in plain sight by the administration and Trump,” Holden wrote. He stressed that premature approval of a vaccine could see a replay of the hydroxychloroquine ‘fiasco’ but the stakes were much higher because of existing fears about vaccines. - Non-invasive ventilation using a firm-fitting face mask can be considered for COVID-19 patients with hypoxaemia who are in negative pressure rooms, according to the latest update from Australia’s National COVID-19 Clinical Evidence Taskforce.
However the advice comes with an emphasis that it should be used with caution and with ‘strict attention’ paid to the safety of staff. - Children have accounted for just over 1% of all COVID-19 cases reported in the UK from January to May, according to a paper published in the Archives of Disease in Childhood.
Of 540,305 people who tested positive for SARS-CoV-2 in England during that period, 1.1% were aged under 16 years, with the median age of childhood cases being 5.9 years.
Among the 1408 cases there were eight deaths, four of which were directly attributed to COVID-19 and three of those were in children with multiple comorbidities.
The authors pointed out that the positivity rate among children tested for SARS-CoV-2 was only 4% – significantly lower than the 50% seen in adults aged 80 years and over.
“Consistent with other countries, children account for a very small proportion of confirmed cases and have very low case-fatality rates,” they wrote. - NSW Health has issued a public health alert for Liverpool Hospital in south-west Sydney, after confirming a third infected staff member at the hospital. The first case was linked to a known cluster, but since then two more staff have tested positive for COVID-19.
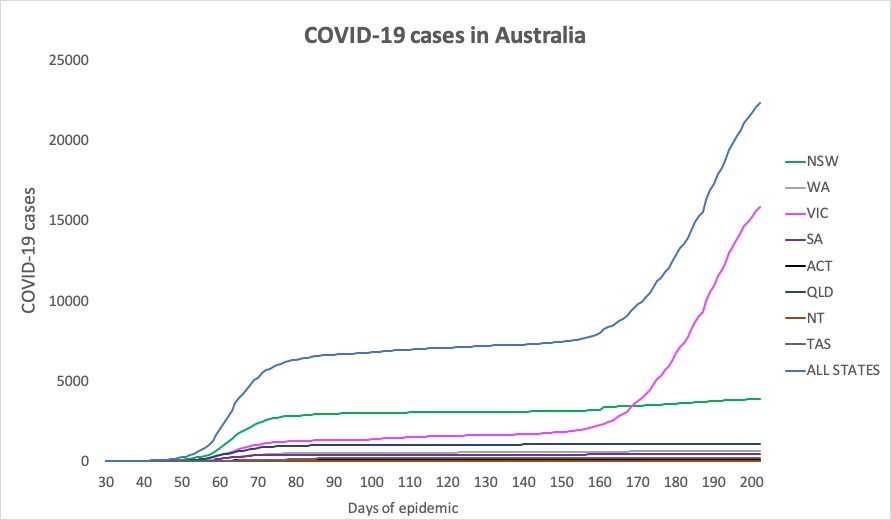
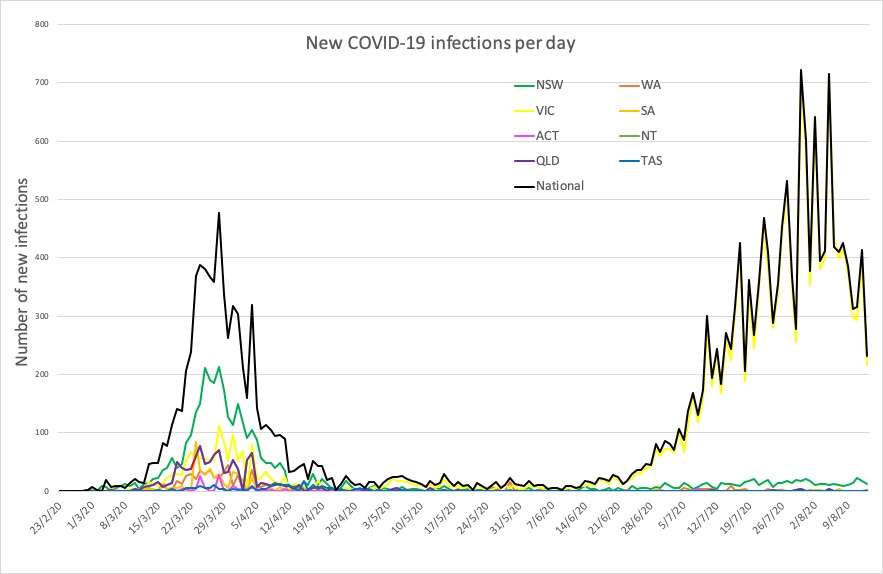
- Here are today’s confirmed COVID-19 infection numbers around Australia to 9pm Thursday, with new case numbers in brackets (and we’re relieved to see the overall infection numbers starting to level off in the charts below):
National – 22,358, with 361 deaths and 686 hospitalised.
ACT – 113
NSW – 3927 (12)
NT – 33 (0)
QLD – 1089 (0)
SA – 459 (0)
TAS – 230 (0)
VIC – 15,863 (278)
WA – 644 (2)