A large new study has shown no benefit in these patients.
Every year, 60,000 people in the UK are diagnosed with heart failure, and many are treated with stents. In a large new study published in the New England Journal of Medicine, my colleagues and I discovered that these procedures are unnecessary.
Heart failure is where the heart muscle becomes weakened, leading to symptoms of severe breathlessness that may cause premature death. The commonest cause is blocked blood vessels that reduce blood supply to the heart muscle. This is known as coronary artery disease.
A person with heart failure is treated with medication and sometimes with specialised pacemakers. Despite this treatment, many patients die prematurely or are admitted to hospital with worsening symptoms.
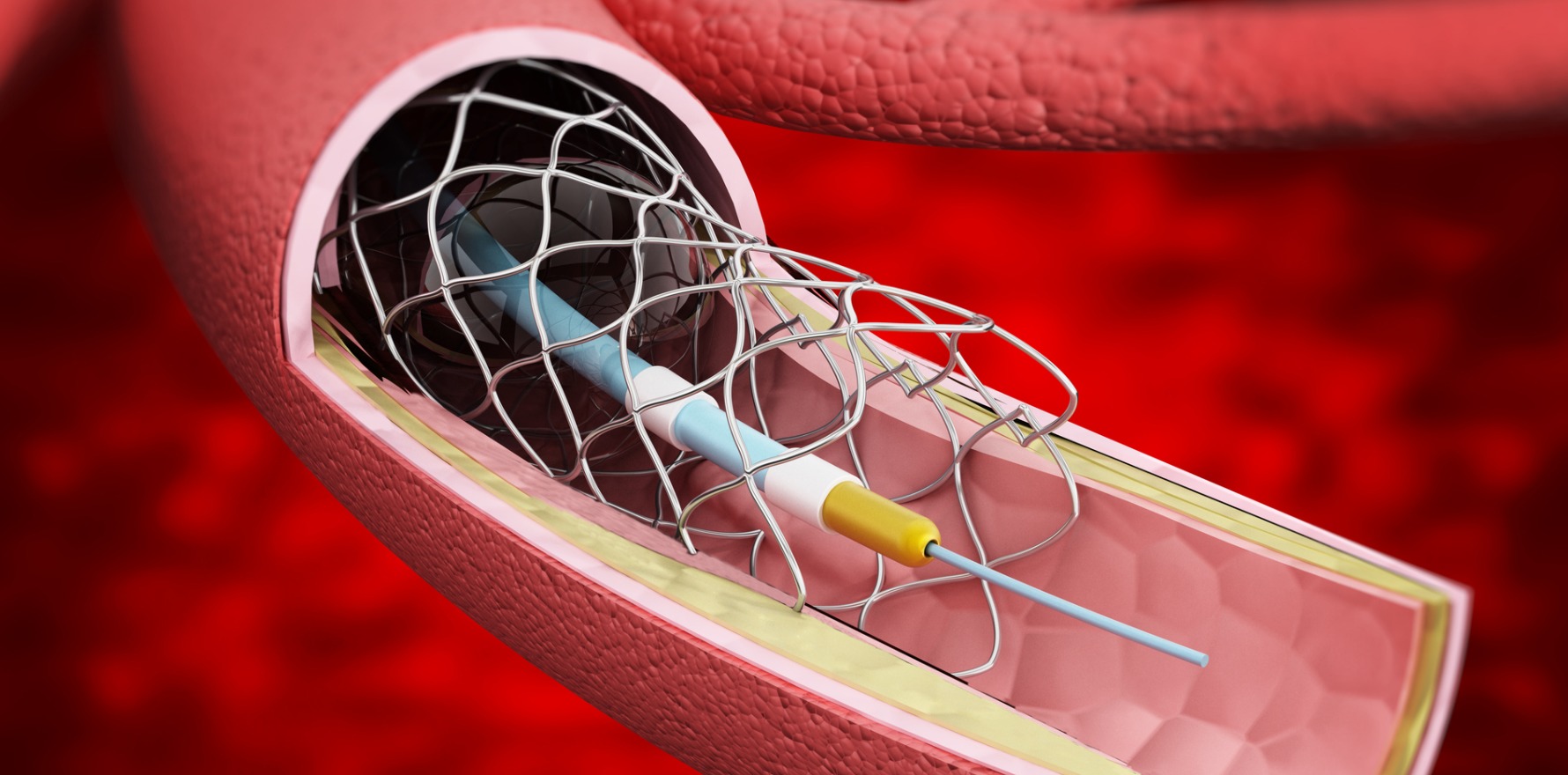
People with heart failure also sometimes have a procedure to insert a stent – a small metal tube that is used to unblock a coronary artery. Stents are placed into the heart arteries by a cardiologist through tubes inserted either into the wrist or the groin and guided by X-rays. Trials have shown that stents are a very effective treatment for people with heart attacks and angina, but their effects in patients with heart failure have remained uncertain.
Some cardiologists had noticed improvements in patients’ symptoms and heart function after stenting, but researchers could not tell if these improvements were directly linked to the stents, or would have happened anyway with medications. Without proper research, treatment guidelines for the use of stents in patients with heart failure varied, with the NHS recommending against stenting and European guidelines recommending it in certain patients.
In this latest study, the REVIVED-BCIS2 trial, led by Professor Divaka Perera, we tested whether treatment with stents helped patients to live longer or to stay out of hospital. The trial was a collaboration of 40 NHS Hospitals in the UK and ran from 2013 to 2020.
Patients could be included in the trial if they had severely weakened heart muscle and extensive blockages of the coronary arteries. They also had specialised heart scans performed, so that stenting could be targeted to the areas of heart muscle that were most likely to recover.
Seven hundred patients took part and half were randomly chosen to receive stents, while all patients received standard heart failure treatment. The patients attended follow-up appointments for up to eight years so that their health and heart function could be monitored closely.
An average of 3.4 years after treatment, patients who received stents were just as likely as those who did not to have died or been admitted to hospital with heart failure, showing that the treatment was not effective.
Heart scans and blood tests also showed no difference in the heart’s pumping strength, supporting the main trial findings.
Our study did show that patients who had stents had a better quality of life in the first year, but after two years the difference disappeared and patients reported similar health. Although there was no benefit to inserting stents, there was also no sign that stents caused harm.
More research is not needed
The results of the trial mean that stents should not be used to treat patients with heart failure caused by coronary artery disease unless they have another condition, such as angina or a recent heart attack.
The design and the number of patients involved in the trial mean the answer is clear and further research to address this question is not needed at the moment. We will spend time looking at the results to try to understand why stenting did not work. Though no benefit was shown, the findings are important as they mean patients with heart failure will not undergo unnecessary procedures. The cost of stenting procedures can also be redirected to providing other treatments and better care for patients with heart failure.
Matthew Ryan, Clinical Lecturer, King’s College London
This article is republished from The Conversation under a Creative Commons licence. Read the original article.