X-ray, CT and MRI all played a role in diagnosing a hot, red, swollen but painless toe.
HISTORY
A 67-year-old man had cut his second toe four weeks prior to presenting with a hot, red, swollen but painless toe. He had a long history of non-insulin dependent type 2 diabetes. On examination, there was an erythematous and swollen distal phalanx with ulceration and purulent discharge and cellulitis.
The initial clinical concern was that of peripheral neuropathy and underlying possible osteomyelitis.
IMAGE FINDINGS
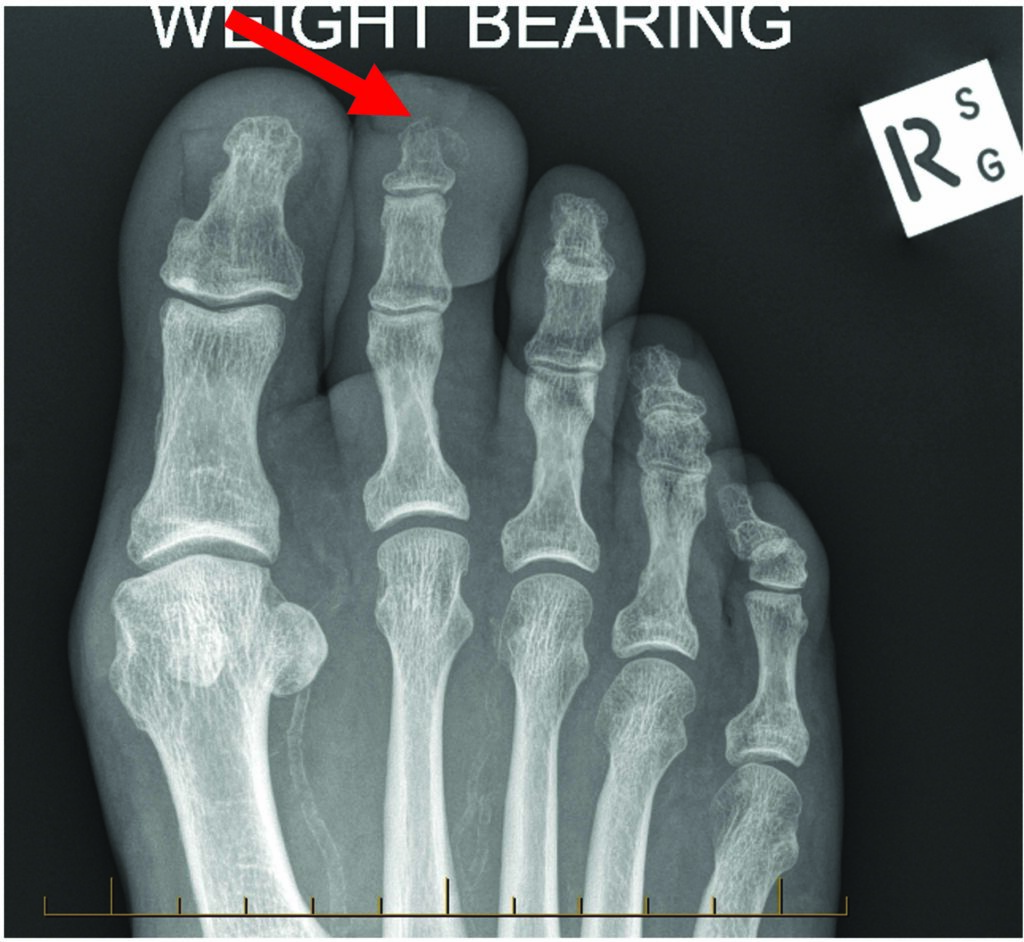
First-line imaging included radiographs of the foot, which revealed an apparent lucency of the cortex of the distal phalanx with surrounding soft tissue thickening. A subsequent CT confirmed the presence of bony destruction of the distal tuft of the second toe, but no sequestrum (devitalised fragment of bone) or periosteal reaction.

Both the X-rays and CT are sensitive at assessing bony destruction which can be seen in late osteomyelitis, but not so much at detecting septic arthritis, abscess formation or early osteomyelitis.
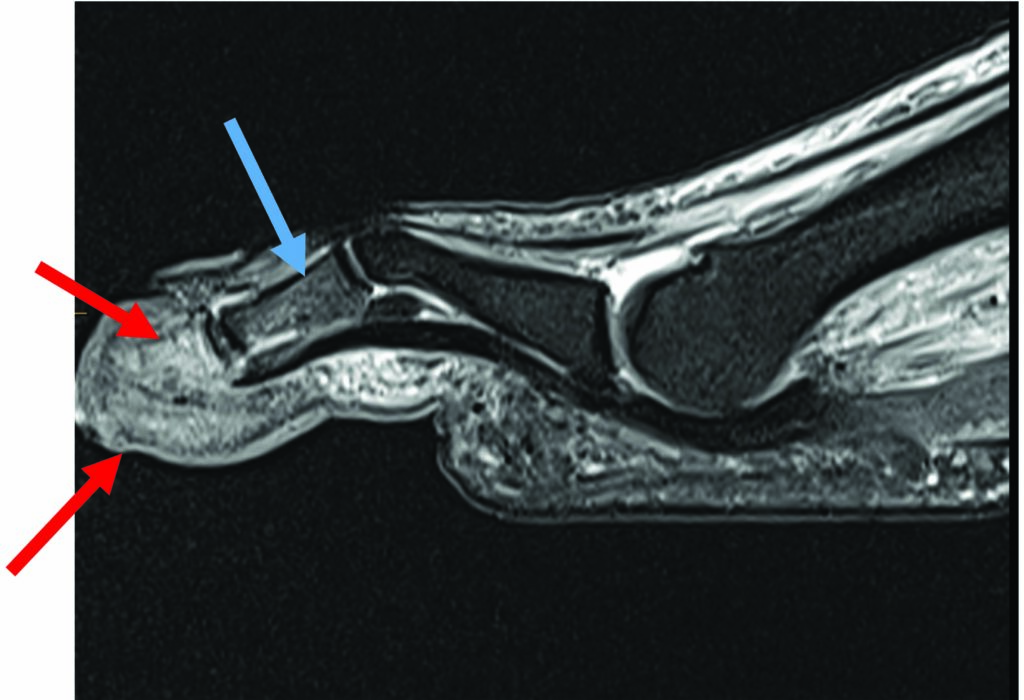
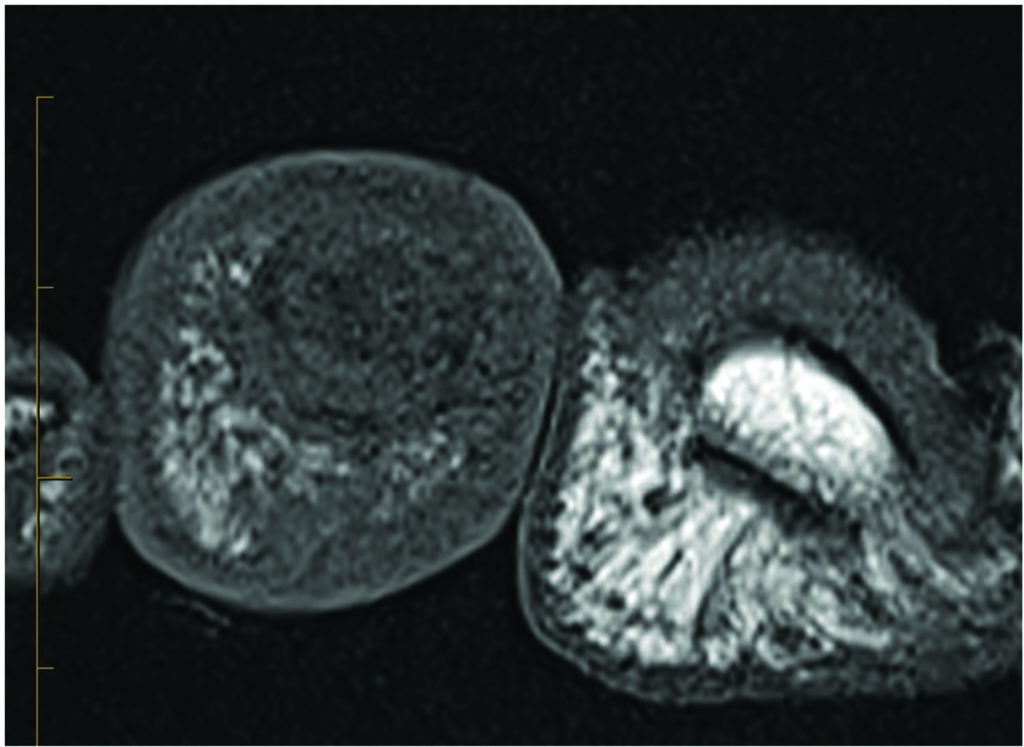
An MRI of this region demonstrated an intensely enhancing marrow in the distal phalanx, with mild enhancement of the intermediate phalanx, but no effusion or periosteal lifting.
Also, low signal in the marrow on the T1 sequence within the distal phalanx is confirmatory of osteomyelitis, but this was not present in the intermediate phalanx.
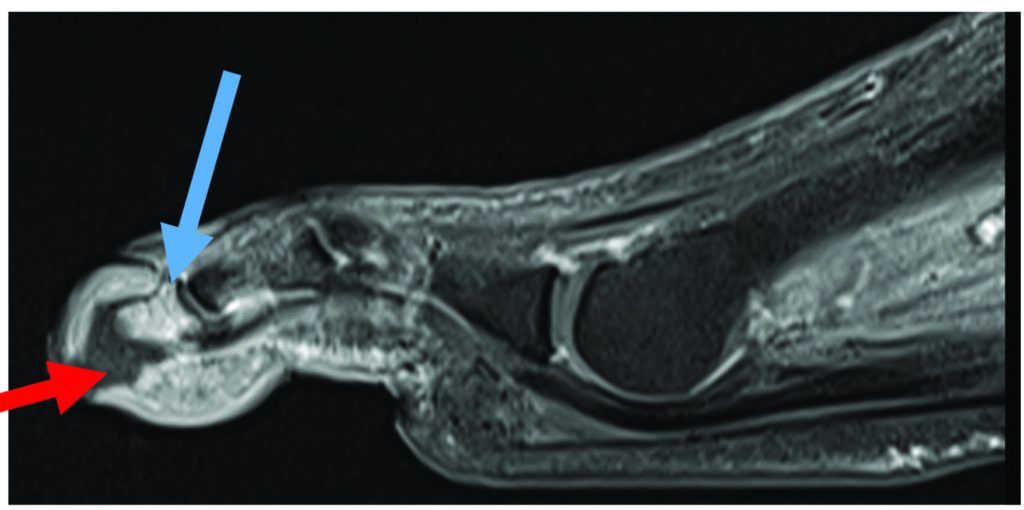
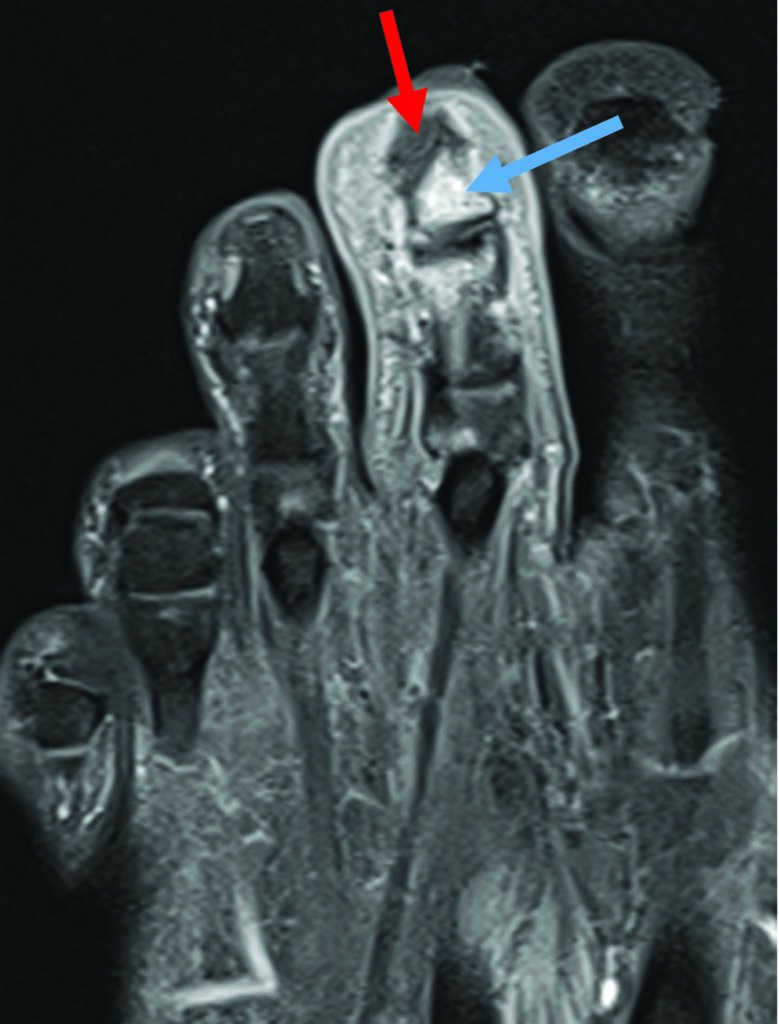
In addition, there is diffuse cellulitis in the soft tissues with a tract of non-enhancing tissue representing an infected sinus tracking from the skin to the bone of the distal phalanx.
DIAGNOSIS
Therefore, the diagnosis was a diabetic infected ulcer with a sinus tract extending into the distal phalanx, causing distal phalanx osteomyelitis, but no septic arthritis. There is reactive oedema without osteomyelitis in the intermediate phalanx. Confidence in this diagnosis was the result of the combination of imaging modalities, in particular the CT and MRI.
MANAGEMENT
Management was amputation of the distal phalanx with resection including the distal interphalangeal joint. The diagnosis, including the absence of septic arthritis in the joint, was confirmed at the time of surgery.
Dr Sebastian Fung is a musculoskeletal radiologist who undertook an MRI imaging fellowship in Hospital for Special Surgery in New York. He now works in Sydney at St Vincent’s Private Hospital and Mater Hospital


